Prednisone offers rapid relief from severe asthma symptoms, reducing airway inflammation and improving breathing within hours. However, it’s a short-term solution, not a long-term management strategy, and prolonged use carries significant side effects.
Doctors typically prescribe prednisone for asthma exacerbations requiring immediate symptom control. Oral doses vary depending on the severity of the attack and patient factors, usually ranging from 20-60 mg daily. Close monitoring by your physician is vital throughout treatment, allowing adjustments based on individual responses.
Common side effects include increased appetite, weight gain, mood changes, and insomnia. More serious risks include elevated blood sugar, increased susceptibility to infections, and bone thinning with extended use. Discuss these potential effects with your doctor to mitigate risks and understand potential alternatives.
Always follow your doctor’s instructions precisely. Never abruptly stop taking prednisone; gradual tapering under medical supervision is necessary to avoid potential complications. Remember, prednisone manages symptoms; a long-term asthma action plan, including inhalers and potentially other medications, is critical for ongoing control and prevention of future attacks. Regular check-ups with your doctor are vital to optimizing your treatment.
For long-term asthma management, your doctor will likely recommend a combination of preventative medications and quick-relief inhalers tailored to your specific needs. This approach provides better overall control and minimizes reliance on steroids like prednisone.
- Asthma Treatment with Prednisone
- Prednisone’s Role in Asthma Management
- Short-Term vs. Long-Term Prednisone Use in Asthma
- Short-Term Prednisone: Benefits and Considerations
- Long-Term Prednisone: Risks and Alternatives
- Common Side Effects of Prednisone for Asthma
- Managing Prednisone Side Effects: Practical Tips
- Dietary Adjustments
- Lifestyle Modifications
- Addressing Specific Side Effects
- When to Contact Your Doctor
- Important Note
- When to Consult a Doctor About Prednisone for Asthma
- When to Discuss Prednisone Usage with Your Doctor
- Alternative Asthma Treatments and Prednisone’s Place in a Comprehensive Plan
Asthma Treatment with Prednisone
Prednisone, a corticosteroid, reduces airway inflammation, a key factor in asthma attacks. It’s a powerful medication, but it’s not a long-term solution.
Doctors prescribe prednisone for asthma exacerbations, offering quick relief from severe symptoms. This includes shortness of breath, wheezing, and coughing.
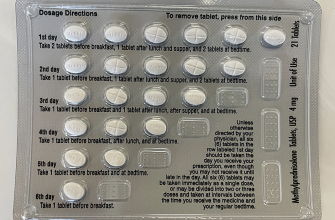
- Short-term use: Prednisone typically works within hours to days, significantly improving lung function. A typical course lasts 5-10 days.
- Dosage: Your doctor determines the correct dosage based on your specific needs. Never adjust your dosage without consulting them.
- Side effects: While beneficial, prednisone can cause side effects such as increased appetite, weight gain, mood changes, and insomnia. These are usually temporary and subside after you stop taking the medication.
Prednisone is usually taken orally, following your doctor’s instructions. It’s vital to complete the entire course, even if your symptoms improve. Stopping early can lead to a relapse.
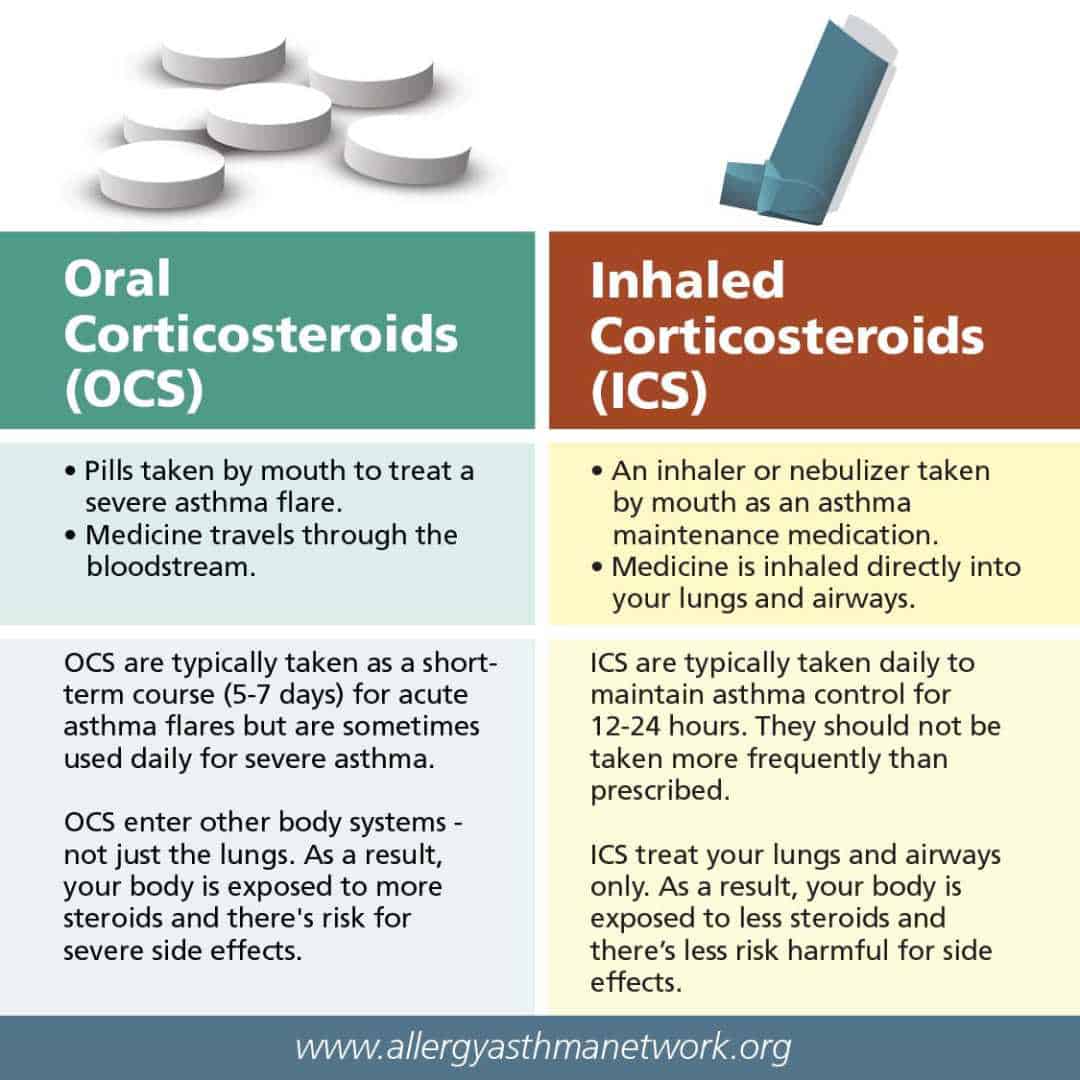
Prednisone is not a preventative medication. To manage asthma long-term, you need a daily controller medication, like inhaled corticosteroids, and a rescue inhaler for quick symptom relief during attacks.
- Inhaled Corticosteroids: These reduce inflammation and prevent asthma attacks. Examples include fluticasone and budesonide.
- Rescue Inhaler: This is a fast-acting bronchodilator, like albuterol, used to relieve sudden symptoms.
Regular check-ups with your doctor are crucial for monitoring your asthma and adjusting your treatment plan as needed. Open communication with your doctor ensures you receive the best care.
Always discuss any concerns or questions you have regarding prednisone or your asthma management with your healthcare provider. They can tailor a treatment plan that’s right for you.
Prednisone’s Role in Asthma Management
Prednisone, a corticosteroid, serves as a powerful anti-inflammatory medication for asthma exacerbations. It reduces airway inflammation, relieving symptoms like wheezing, coughing, and shortness of breath quickly.
Doctors prescribe prednisone for short-term use during severe asthma attacks or when other treatments prove insufficient. A typical course involves several days of oral medication, with the dosage gradually decreasing to minimize side effects.
While highly effective, prolonged prednisone use carries risks. These include increased blood sugar, weight gain, bone thinning, and mood changes. Therefore, adherence to prescribed dosages and duration is paramount.
Your doctor will carefully monitor your condition while you are on prednisone. Regular blood tests may be necessary to track potential side effects and assess the treatment’s efficacy. They will also work with you to develop a long-term asthma management plan that minimizes reliance on prednisone.
Remember, prednisone is not a cure for asthma; it’s a powerful tool for managing flare-ups. Combining prednisone with a regular asthma controller medication, such as an inhaled corticosteroid, provides the best overall control and minimizes the need for future prednisone treatments.
Always discuss any concerns about prednisone with your healthcare provider. They can address your questions, explain potential side effects, and tailor the treatment plan to your specific needs.
Short-Term vs. Long-Term Prednisone Use in Asthma
Prednisone’s role in asthma management hinges heavily on the duration of its use. Short-term prednisone courses, typically lasting a few days to a week, effectively control severe asthma flare-ups. This quick action reduces inflammation and airway narrowing, providing rapid relief. However, long-term prednisone use carries significant risks.
Short-Term Prednisone: Benefits and Considerations
Short bursts are generally safe for managing acute exacerbations. Benefits include rapid symptom improvement. However, remember that frequent short courses signal underlying asthma control issues needing addressing through other methods, such as long-term controller medications (inhalers).
Long-Term Prednisone: Risks and Alternatives
Prolonged prednisone use is strongly discouraged due to severe side effects. These include weight gain, high blood pressure, osteoporosis, increased risk of infections, cataracts, and glaucoma. Long-term prednisone is rarely the best approach for asthma management. Instead, prioritize well-managed daily controller medications, like inhaled corticosteroids or long-acting beta-agonists. These provide sustained control, minimizing the need for prednisone altogether.
| Prednisone Use | Duration | Benefits | Risks |
|---|---|---|---|
| Short-term | Days to a week | Rapid symptom relief | Minimal, if used appropriately |
| Long-term | Weeks or months | None outweigh the risks | Significant; weight gain, high blood pressure, osteoporosis, increased infections, cataracts, glaucoma |
Always discuss prednisone use with your doctor. They’ll assess your asthma and recommend the best treatment plan, balancing benefits and potential harms. Focus on proactive asthma management to minimize reliance on prednisone.
Common Side Effects of Prednisone for Asthma
Prednisone offers significant relief for asthma symptoms, but it’s crucial to understand potential side effects. Many are manageable, and some disappear once you stop taking the medication. However, awareness is key.
Weight gain is a frequent side effect. Prednisone can increase appetite and cause fluid retention. Maintain a healthy diet and engage in regular physical activity to mitigate this. Consult your doctor about dietary adjustments.
Increased blood sugar is another common concern, especially for individuals with pre-existing diabetes. Regular blood sugar monitoring is advised. Your doctor may adjust your diabetes medication accordingly.
Mood changes, ranging from irritability to anxiety and even depression, can occur. Open communication with your doctor is vital. They can offer support and explore alternative treatments if needed.
Insomnia and difficulty sleeping affect some patients. Establish a consistent sleep schedule and maintain a relaxing bedtime routine. Avoid caffeine and alcohol before bed.
High blood pressure can be a side effect. Regular blood pressure checks are necessary. Your doctor might prescribe medication to manage this.
Muscle weakness and bone thinning (osteoporosis) are long-term risks with prolonged prednisone use. Weight-bearing exercise and a calcium-rich diet can help mitigate these effects. Discuss bone density testing with your doctor.
Gastrointestinal issues such as heartburn, stomach upset, and ulcers are possible. Taking prednisone with food can lessen digestive problems. Inform your doctor immediately if you experience severe stomach pain.
Remember, this list doesn’t include every possible side effect. Always discuss any concerns or new symptoms with your doctor or pharmacist. They can help you manage side effects and ensure your asthma treatment remains safe and effective.
Managing Prednisone Side Effects: Practical Tips
Drink plenty of water throughout the day to stay hydrated and help your body process the medication. This simple step can significantly reduce feelings of dryness and fatigue.
Dietary Adjustments
Focus on a balanced diet rich in potassium. Good sources include bananas, sweet potatoes, and spinach. This helps counteract potential potassium loss caused by prednisone.
- Limit your sodium intake to reduce water retention.
- Choose lean protein sources and whole grains for sustained energy.
- Increase your calcium intake via dairy products or supplements to support bone health.
Lifestyle Modifications
Regular, gentle exercise, such as walking or swimming, can help manage weight gain and improve mood. Always check with your doctor before starting any new exercise routine.
- Prioritize sufficient sleep. Aim for 7-8 hours of quality sleep each night.
- Manage stress through relaxation techniques like deep breathing or meditation.
- Monitor your blood sugar regularly, especially if you have diabetes, as prednisone can affect blood sugar levels.
Addressing Specific Side Effects
If you experience insomnia, avoid caffeine and alcohol before bed. Try establishing a relaxing bedtime routine.
- For increased appetite, eat smaller, more frequent meals to avoid overeating.
- Report any significant mood changes to your doctor immediately.
- Use a moisturizer to combat dry skin.
When to Contact Your Doctor
Contact your healthcare provider immediately if you experience severe side effects such as severe mood swings, significant weight gain, or vision changes.
Important Note
This information is for guidance only and does not replace professional medical advice. Always discuss your treatment plan and any concerns with your doctor.
When to Consult a Doctor About Prednisone for Asthma
Contact your doctor immediately if you experience any serious side effects. These include severe mood changes (like unusual irritability or depression), rapid weight gain, muscle weakness, increased thirst or urination, vision problems, or swelling in your face or legs. Don’t hesitate – prompt medical attention is critical.
When to Discuss Prednisone Usage with Your Doctor
Schedule a consultation if your asthma symptoms aren’t well-controlled despite using your inhalers correctly. Similarly, talk to your physician if you need to use your rescue inhaler more frequently than usual. Regular check-ups to monitor your condition and adjust your medication are recommended, especially if you’re on a long-term prednisone course. This ensures your treatment remains appropriate and minimizes potential side effects. Discuss any concerns about prednisone side effects; your doctor can assess your specific situation and make informed adjustments to your treatment plan.
Remember, open communication with your doctor is crucial for managing your asthma effectively and safely. Always report any new or worsening symptoms.
Alternative Asthma Treatments and Prednisone’s Place in a Comprehensive Plan
Prednisone, a powerful corticosteroid, effectively controls severe asthma flare-ups. However, long-term use carries risks. A holistic approach integrates prednisone with other therapies to minimize side effects and maximize control.
Inhaled corticosteroids (ICS) form the cornerstone of long-term asthma management. They reduce inflammation directly in the lungs, offering superior long-term benefits compared to prednisone’s systemic effects. Daily use is common, with dosages adjusted to individual needs.
Long-acting beta-agonists (LABAs), combined with ICS, provide additional bronchodilation, further improving lung function. This combination proves especially beneficial for patients with persistent symptoms.
Biologics offer targeted therapy for specific asthma types, often those resistant to standard treatment. These medications precisely target inflammatory pathways, offering relief for severe, hard-to-treat asthma. Discuss suitability with your doctor.
Leukotriene modifiers help reduce inflammation and bronchoconstriction, proving useful in combination with other therapies. They can provide additional control for many patients.
Allergen avoidance strategies, such as eliminating pet dander or managing dust mites, represent crucial preventative steps, reducing the need for medication.
Breathing techniques, like diaphragmatic breathing, can help improve lung capacity and reduce breathlessness, offering self-managed relief for mild symptoms.
Prednisone’s role lies in managing acute exacerbations and severe inflammation when other therapies are insufficient. It acts quickly to reduce inflammation, preventing serious complications. Your physician will tailor the duration and dosage.
Remember: This information doesn’t replace professional medical advice. Consult your doctor to develop a personalized asthma management plan. Regular monitoring, including peak flow measurements, is vital for tracking progress and adjusting treatment as needed.