Yes, prednisone use is associated with an increased risk of atrial fibrillation (AFib). Studies show a statistically significant link, although the exact mechanism isn’t fully understood. This increased risk is particularly relevant for patients already predisposed to heart rhythm problems or those on concurrent medications that might exacerbate the effect.
The risk isn’t uniform; factors like dosage, duration of prednisone treatment, and individual patient characteristics influence the likelihood of developing AFib. Higher doses and longer treatment periods appear to correlate with a greater risk. Pre-existing conditions such as hypertension, diabetes, and obstructive sleep apnea amplify this risk considerably.
Therefore, open communication with your doctor is crucial. Discuss your concerns regarding AFib if you’re prescribed prednisone, especially if you have a personal or family history of heart problems. Regular monitoring of your heart rhythm during and after prednisone therapy might be recommended, particularly with high-dose or long-term use. This could involve electrocardiograms (ECGs) or other cardiac assessments.
Remember, this information serves for educational purposes only and does not replace professional medical advice. Always consult your physician before making any decisions regarding your medication or healthcare.
- Can Prednisone Cause Atrial Fibrillation?
- Prednisone’s Mechanism of Action and its Impact on the Heart
- Evidence Linking Prednisone Use to Atrial Fibrillation Risk
- Specific Prednisone Dosage and Duration Affecting Atrial Fibrillation Risk
- Dosage-Specific Risk Stratification
- Duration-Dependent Risk Considerations
- Identifying Predisposing Factors that Increase Risk with Prednisone Use
- Recognizing Symptoms of Atrial Fibrillation While on Prednisone
- Common AFib Symptoms
- Less Common, But Still Important, Symptoms
- How Prednisone Might Affect Symptoms
- When to Seek Immediate Medical Attention
- Tracking Your Symptoms
- Managing Atrial Fibrillation Risk During and After Prednisone Treatment
- Minimizing Risk During Treatment
- Post-Prednisone Management
- Monitoring Your Heart Health After Prednisone
Can Prednisone Cause Atrial Fibrillation?
Prednisone, while effective for inflammation, can increase your risk of atrial fibrillation (AFib). This risk is linked to several factors, including the dose and duration of prednisone treatment.
Higher doses and longer treatment periods correlate with a greater likelihood of developing AFib. This is because prednisone affects electrolyte balance, particularly potassium levels, which are crucial for maintaining a regular heartbeat. Electrolyte imbalances can disrupt the heart’s electrical signals, increasing the chance of irregular rhythms, including AFib.
Other risk factors for AFib, such as age, hypertension, and underlying heart conditions, significantly compound the risk when combined with prednisone use. Individuals with pre-existing heart conditions should discuss the potential risks with their physician before starting prednisone.
Regular monitoring of heart rate and rhythm is recommended for patients taking prednisone, especially those with risk factors for AFib. Your doctor might suggest an electrocardiogram (ECG) to check for any irregularities. Open communication with your healthcare provider is key; promptly reporting any symptoms suggestive of AFib, such as palpitations, shortness of breath, or dizziness, is crucial for timely intervention.
While prednisone can increase AFib risk, it’s not guaranteed to cause it in everyone. The decision to prescribe prednisone should consider the benefits against potential side effects, carefully weighing individual circumstances. Always follow your doctor’s instructions regarding dosage and duration of treatment.
Prednisone’s Mechanism of Action and its Impact on the Heart
Prednisone, a glucocorticoid, works by binding to glucocorticoid receptors within cells. This binding influences gene expression, impacting various bodily processes. Specifically relevant to cardiac function, prednisone can increase the heart’s workload by raising blood pressure and blood sugar. These effects stem from its influence on fluid retention and the body’s metabolism.
Elevated blood pressure, a common side effect, increases the strain on the heart muscle, potentially contributing to atrial fibrillation (AFib). Similarly, increased blood sugar levels can cause damage to blood vessels, further promoting the risk of AFib. Prednisone’s influence on electrolyte balance – particularly potassium levels – also plays a role. Low potassium levels can trigger abnormal heart rhythms, including AFib.
The duration and dosage of prednisone directly correlate with the risk of these cardiovascular effects. Higher doses and prolonged use significantly heighten the chances of developing AFib. Individuals with pre-existing heart conditions are particularly vulnerable. Regular monitoring of blood pressure, blood sugar, and electrolyte levels is crucial while taking prednisone, especially for those with a history of heart problems.
Consult your physician immediately if you experience symptoms of AFib, such as palpitations, shortness of breath, or dizziness, while taking prednisone. They can assess your risk factors, adjust medication, or recommend alternative treatment strategies. Open communication with your doctor is vital for managing potential risks and ensuring your overall health.
Evidence Linking Prednisone Use to Atrial Fibrillation Risk
Studies show a correlation between prednisone use and increased atrial fibrillation (AFib) risk. This isn’t a guaranteed outcome; however, understanding the connection is vital for informed decision-making.
Several mechanisms explain this link:
- Electrolyte Imbalances: Prednisone can disrupt potassium and magnesium levels, crucial for maintaining a regular heartbeat. These imbalances predispose individuals to AFib.
- Fluid Retention: Prednisone can cause fluid retention, increasing the volume of blood the heart pumps. This added strain can trigger AFib.
- Increased Blood Pressure: Prednisone’s effect on fluid balance often leads to elevated blood pressure, a known AFib risk factor.
- Cardiovascular Effects: Some research suggests that prednisone may have direct effects on the heart muscle, increasing susceptibility to irregular rhythms like AFib.
Observational studies have demonstrated a statistically significant increase in AFib incidence among prednisone users compared to non-users. However, the magnitude of this risk varies based on factors like dosage, duration of use, and individual patient characteristics. For example:
- Higher prednisone doses generally correlate with a higher AFib risk.
- Long-term prednisone use presents a greater risk compared to short-term treatment.
- Pre-existing cardiovascular conditions increase the likelihood of AFib development in individuals using prednisone.
While these studies indicate a link, they don’t prove causation. More research is needed to fully understand the complex interplay between prednisone and AFib risk. Regular monitoring of heart rhythm, especially during and after prednisone treatment, is advisable for high-risk individuals.
Consult your physician for personalized advice. They can assess your specific risk factors and determine the best course of action given your health history and current medication.
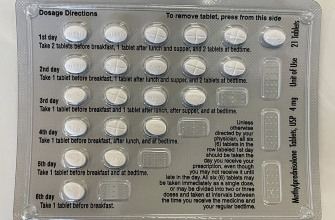
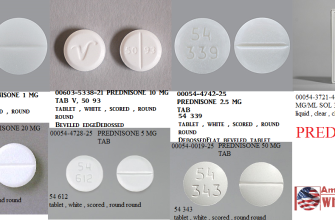
Specific Prednisone Dosage and Duration Affecting Atrial Fibrillation Risk
Higher prednisone doses and longer treatment durations increase atrial fibrillation risk. Studies show a statistically significant correlation between cumulative prednisone dosage exceeding 1000mg and a heightened risk of developing atrial fibrillation. Patients receiving prednisone for more than three months face a considerably greater risk compared to those on shorter courses. This risk is amplified in individuals with pre-existing cardiac conditions or risk factors for atrial fibrillation.
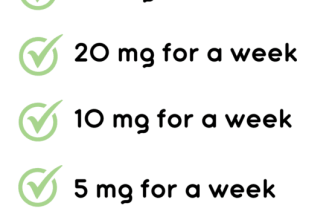
Dosage-Specific Risk Stratification
While precise numbers vary across studies, a meta-analysis suggests a roughly 2-fold increase in atrial fibrillation incidence with cumulative doses exceeding 1000mg. Doses above 40mg daily carry a particularly elevated risk, especially when administered for extended periods. Conversely, lower doses (≤10mg daily) for short periods show less dramatic risk increases, though still present. It’s crucial to weigh the benefits of prednisone against this potential risk on a case-by-case basis.
Duration-Dependent Risk Considerations
The risk of atrial fibrillation isn’t simply dose-dependent; it also grows significantly with longer treatment durations. Beyond three months of continuous prednisone use, the risk profile escalates noticeably. This prolonged exposure to corticosteroids likely contributes to electrolyte imbalances and other physiological changes that predispose individuals to atrial fibrillation. Regular monitoring of cardiac function is highly recommended for patients on long-term prednisone therapy.
Identifying Predisposing Factors that Increase Risk with Prednisone Use
Understanding your individual risk is key. Pre-existing heart conditions significantly elevate your chances of developing atrial fibrillation while on prednisone. This includes conditions like hypertension, coronary artery disease, and previous heart valve problems. Regular monitoring of blood pressure is therefore crucial.
Age plays a role. Older individuals generally face a higher risk, primarily because the aging process often weakens the heart’s electrical system. This makes it more susceptible to arrhythmias, including atrial fibrillation.
A family history of atrial fibrillation increases your susceptibility. Genetic predisposition contributes to a higher likelihood of developing the condition, regardless of medication use.
Underlying health issues beyond heart conditions also matter. Conditions such as diabetes, chronic lung disease, and thyroid disorders can increase your risk of atrial fibrillation, and prednisone may exacerbate these risks.
High doses of prednisone and prolonged treatment durations increase the probability of experiencing adverse cardiac effects. Your doctor should carefully consider the necessary dose and length of treatment.
Lifestyle factors such as obesity, smoking, and excessive alcohol consumption heighten the overall risk. These habits often negatively impact cardiovascular health and should be addressed proactively.
Open communication with your physician is paramount. Discuss your complete medical history, including any family history of heart problems, to allow for a thorough risk assessment and appropriate monitoring during prednisone treatment.
Recognizing Symptoms of Atrial Fibrillation While on Prednisone
Prednisone can increase your risk of atrial fibrillation (AFib). Therefore, it’s crucial to know the symptoms, so you can seek medical attention promptly.
Common AFib Symptoms
The most common symptom is an irregular heartbeat, often described as a fluttering or racing heart. You might feel palpitations – a noticeable thumping or pounding in your chest. Shortness of breath and chest pain can also occur.
Less Common, But Still Important, Symptoms
Fatigue, dizziness, and lightheadedness are other potential indicators. Weakness and fainting are less frequent but warrant immediate medical attention. Note that these symptoms can be associated with other conditions, so don’t self-diagnose.
How Prednisone Might Affect Symptoms
Prednisone’s effect on blood sugar and fluid retention can indirectly exacerbate AFib symptoms. For instance, increased blood sugar might cause intensified palpitations, while fluid retention can lead to shortness of breath.
When to Seek Immediate Medical Attention
Seek immediate medical attention if you experience sudden, severe chest pain, severe shortness of breath, or fainting. Contact your doctor if you notice a persistent irregular heartbeat or significant increase in the frequency or intensity of your symptoms.
Tracking Your Symptoms
| Symptom | Frequency | Severity (1-10) | Date/Time | Notes |
|---|---|---|---|---|
| Irregular Heartbeat | ||||
| Palpitations | ||||
| Shortness of Breath | ||||
| Chest Pain | ||||
| Fatigue | ||||
| Dizziness/Lightheadedness |
Keeping a detailed record of your symptoms can be incredibly helpful for your doctor in diagnosing and managing your condition.
Managing Atrial Fibrillation Risk During and After Prednisone Treatment
Regularly monitor your heart rate and rhythm. Report any palpitations, rapid heartbeat, or shortness of breath to your doctor immediately. This proactive approach is key.
Minimizing Risk During Treatment
- Maintain a healthy lifestyle. This includes regular exercise (as tolerated), a balanced diet low in sodium and saturated fat, and weight management.
- Follow your doctor’s prescribed dosage and duration of prednisone precisely. Avoid self-adjusting your medication.
- If you have pre-existing heart conditions, discuss the risks with your cardiologist before starting prednisone. They may recommend closer monitoring or alternative treatment options.
- Stay hydrated. Dehydration can exacerbate atrial fibrillation.
Post-Prednisone Management
Your risk of atrial fibrillation may decrease once you finish prednisone, but continued vigilance is necessary.
Monitoring Your Heart Health After Prednisone
- Schedule a follow-up appointment with your doctor to discuss any lingering symptoms or concerns.
- Continue to maintain a healthy lifestyle. These habits contribute to long-term heart health.
- Your doctor may recommend continuing heart rate and rhythm monitoring, depending on your individual situation and medical history.
- Learn the signs and symptoms of atrial fibrillation and seek prompt medical attention should they occur.
Remember, open communication with your healthcare team is critical for managing your health effectively. Don’t hesitate to ask questions and share your concerns.