Prednisone can sometimes cause a cough as a side effect. This isn’t uncommon, and often resolves itself as your body adjusts to the medication. However, understanding the potential causes and appropriate responses is key to managing this symptom effectively.
A dry, persistent cough is a common complaint among prednisone users. This is frequently linked to the medication’s impact on the mucous membranes, leading to irritation and subsequent coughing. Drinking plenty of fluids can help alleviate dryness. If the cough becomes severe or persistent, consider contacting your doctor. They can evaluate the situation and adjust your treatment plan if necessary.
In some instances, the cough might signify a more serious underlying condition, particularly if accompanied by other symptoms like fever, shortness of breath, or chest pain. Prompt medical attention is necessary in these scenarios. Your doctor can perform tests to rule out infections or other complications unrelated to prednisone.
Remember: This information is for general knowledge and should not replace professional medical advice. Always consult your physician or pharmacist regarding any concerns about medication side effects. They can provide tailored recommendations based on your individual health history and current treatment.
- Cough on Prednisone: A Comprehensive Guide
- Understanding Prednisone-Induced Cough
- Managing Your Cough
- When to Seek Immediate Medical Attention
- Understanding Prednisone and its Side Effects
- Common Side Effects
- Less Common, but Serious Side Effects
- Managing Side Effects
- Common Causes of Cough Related to Prednisone
- Differentiating Prednisone Cough from Other Illnesses
- Prednisone-Induced Cough Characteristics
- Cough Due to Other Illnesses
- Identifying Other Illnesses
- When to Seek Medical Attention for a Prednisone-Induced Cough
- Severe Cough Symptoms Requiring Immediate Medical Attention
- When to Schedule an Appointment with Your Doctor
- Managing a Cough While on Prednisone: Home Remedies
- Saline Nasal Rinse
- Over-the-Counter Remedies
- Lifestyle Adjustments
- When to See a Doctor
- Helpful Chart: Comparing Home Remedies
- Medication Options for Treating Prednisone-Related Cough
- Addressing Underlying Causes
- Managing Symptoms
- Preventing Prednisone-Induced Cough
- Managing Underlying Conditions
- Long-Term Effects and Considerations
- Bone Health
- Glucose Metabolism
- Other Potential Side Effects
- Tapering Off Prednisone
- Regular Monitoring
- Lifestyle Adjustments for Cough Relief During Prednisone Treatment
- Managing Your Surroundings
- Dietary Considerations
- Other Strategies
- When to Seek Medical Attention
Cough on Prednisone: A Comprehensive Guide
Prednisone can cause a cough, often a dry, persistent one. This usually isn’t a serious infection, but it’s uncomfortable. If your cough develops after starting prednisone, contact your doctor. They can assess if the cough stems from prednisone or another cause.
Understanding Prednisone-Induced Cough
Prednisone suppresses the immune system. This can lead to increased mucus production or make you more susceptible to viral infections, resulting in a cough. The cough’s severity varies, some experience a mild tickle, others a persistent hacking cough. The duration also differs, often resolving once you reduce or stop prednisone.
Managing Your Cough
Your doctor might suggest over-the-counter remedies like cough suppressants or expectorants depending on your cough type (dry or productive). Increasing fluid intake helps thin mucus. A humidifier can soothe irritated airways. Avoid irritants like smoke or dust. Remember, self-treating isn’t always best; always consult your physician for guidance.
When to Seek Immediate Medical Attention
Seek immediate medical help if your cough is accompanied by shortness of breath, chest pain, fever, or green/yellow phlegm, as these might indicate a more serious condition like pneumonia or bronchitis requiring immediate treatment. These symptoms could indicate a secondary infection that needs specific antibiotics.
Understanding Prednisone and its Side Effects
Prednisone is a powerful corticosteroid, often prescribed for inflammation. However, it comes with potential side effects. Understanding these side effects helps manage them effectively.
Common Side Effects
- Increased appetite and weight gain: Monitor your calorie intake and consider regular exercise to mitigate this.
- Mood changes: These range from mild irritability to more significant mood swings. Communicate openly with your doctor if you experience these.
- Fluid retention: This can lead to swelling in your face, legs, or ankles. Reduce sodium intake in your diet.
- High blood sugar: Regular blood sugar monitoring is important, especially if you have diabetes. Your doctor might adjust your diabetes medication.
- Increased risk of infection: Prednisone weakens your immune system. Practice good hygiene and avoid contact with sick individuals.
Less Common, but Serious Side Effects
While less frequent, certain side effects require immediate medical attention:
- Severe allergic reactions: Symptoms include hives, swelling of the face or throat, difficulty breathing.
- Muscle weakness: This can increase the risk of falls and fractures. Exercise cautiously and discuss this with your doctor.
- Osteoporosis: Long-term use increases bone loss. Discuss preventative measures like calcium and Vitamin D supplements with your doctor.
- Glaucoma or cataracts: Regular eye exams are crucial during prednisone treatment.
- Stomach ulcers: Your doctor may prescribe medication to protect your stomach lining.
Managing Side Effects
Successfully managing side effects often involves a collaborative approach with your healthcare provider. They can adjust your dosage, prescribe additional medications, and offer lifestyle recommendations to minimize negative impacts. Open communication is key.
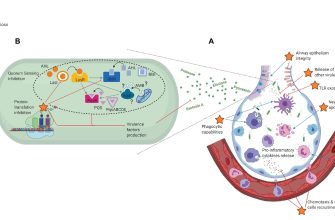
Common Causes of Cough Related to Prednisone
Prednisone, while effective for inflammation, can trigger a cough through several mechanisms. One common reason is increased susceptibility to infections. Prednisone weakens the immune system, making you more vulnerable to respiratory infections like bronchitis or pneumonia, which often manifest as a cough.
Another factor is increased mucus production. Prednisone can sometimes thicken the mucus in your airways, leading to a persistent cough as your body tries to clear the airways. This can be particularly noticeable in individuals with pre-existing respiratory conditions like asthma or COPD.
A less frequent but potential cause is a direct effect on the airways. Some individuals experience airway irritation or inflammation due to prednisone itself, resulting in a cough. This is less common, but it’s a possibility.
Finally, underlying conditions worsened by prednisone, such as GERD (Gastroesophageal reflux disease), can also lead to a cough. Acid reflux can irritate the throat and trigger coughing.
If you experience a cough while taking prednisone, consult your doctor. They can determine the underlying cause and suggest appropriate management strategies, potentially including adjustments to your medication or treatment for the underlying condition. Do not self-treat.
Differentiating Prednisone Cough from Other Illnesses
A cough while on prednisone can be tricky! It might be a side effect of the medication itself, or something entirely separate. Let’s clarify how to tell the difference.
Prednisone-Induced Cough Characteristics
- Timing: Typically appears within a few days to weeks of starting prednisone.
- Type: Often a dry, non-productive cough, meaning it doesn’t produce mucus.
- Severity: Can range from mild to moderate; rarely severe.
- Other symptoms: May be accompanied by other prednisone side effects like increased thirst, weight gain, or mood changes. Absence of fever or other respiratory symptoms is also common.
If your cough matches this description, talk to your doctor. They might adjust your dosage or prescribe additional medication to manage the cough.
Cough Due to Other Illnesses
Many illnesses cause coughs. Distinguishing them is crucial for proper treatment. Here’s a checklist:
Identifying Other Illnesses
- Respiratory Infections (e.g., colds, flu, bronchitis, pneumonia): These coughs often produce mucus (phlegm), may be accompanied by fever, chills, body aches, and congestion. Your doctor can diagnose these with a physical exam and possibly a chest X-ray.
- Allergies: Allergic coughs are often accompanied by sneezing, runny nose, itchy eyes, and other allergy symptoms. An allergist can perform tests to identify specific allergens.
- Gastroesophageal reflux disease (GERD): A chronic cough can sometimes result from stomach acid refluxing into the esophagus. Heartburn and indigestion are common alongside the cough. A gastroenterologist can diagnose and manage GERD.
- Asthma: Wheezing, shortness of breath, and chest tightness accompany asthma coughs. A pulmonologist or allergist can diagnose asthma.
Remember, self-diagnosing can be inaccurate. Always consult your doctor if you have concerns about your cough, particularly while taking medication like prednisone. They can provide the most accurate diagnosis and appropriate treatment plan.
When to Seek Medical Attention for a Prednisone-Induced Cough
Contact your doctor immediately if your cough is severe, accompanied by shortness of breath, or worsens despite taking prednisone.
Severe Cough Symptoms Requiring Immediate Medical Attention
- Cough producing significant amounts of thick mucus.
- Cough that interferes with sleep or daily activities.
- Wheezing or whistling sounds during breathing.
- Chest pain or tightness.
- High fever (over 100.4°F or 38°C).
- Bluish discoloration of the lips or fingertips (cyanosis).
These symptoms may indicate a serious underlying condition requiring prompt medical intervention. Don’t delay seeking help; early treatment is vital for better outcomes.
When to Schedule an Appointment with Your Doctor
- Persistent cough lasting longer than two weeks, even if mild.
- Cough accompanied by a persistent headache or fatigue.
- Cough that causes you to feel generally unwell.
- Worsening of pre-existing lung conditions like asthma or COPD while taking prednisone.
- New onset of cough while on prednisone, especially if you have a history of lung problems.
Scheduling an appointment allows your doctor to assess your condition and adjust your treatment plan if needed. Open communication with your healthcare provider is key to managing your symptoms effectively.
Managing a Cough While on Prednisone: Home Remedies
Drink plenty of fluids, especially warm liquids like broth or tea with honey (honey can soothe a sore throat). This helps thin mucus and ease coughing.
Use a humidifier or take a hot shower. The added moisture in the air can loosen congestion and reduce cough severity.
Rest is crucial. Your body needs time to heal. Get adequate sleep to support your immune system.
Saline Nasal Rinse
A saline nasal rinse can help clear nasal passages, reducing post-nasal drip, a common cough trigger. You can buy pre-made saline sprays or create your own solution with distilled water and salt.
Over-the-Counter Remedies
Consider over-the-counter cough suppressants or expectorants. Always follow dosage instructions and consult a pharmacist or doctor if you have questions or concerns.
Lifestyle Adjustments
Avoid irritants like smoke and dust. These can exacerbate cough symptoms. Also, try to minimize exposure to allergens, if applicable.
When to See a Doctor
If your cough worsens, persists for an extended period, or is accompanied by other symptoms like fever or shortness of breath, seek medical attention immediately.
Helpful Chart: Comparing Home Remedies
| Remedy | Benefits | Considerations |
|---|---|---|
| Hydration (fluids) | Thins mucus, soothes throat | Avoid excessive caffeine or alcohol |
| Humidifier/Shower | Adds moisture to air, loosens congestion | Ensure humidifier is clean to prevent mold growth |
| Rest | Allows body to heal, boosts immune system | Aim for 7-8 hours of sleep per night |
| Saline rinse | Clears nasal passages, reduces post-nasal drip | Use distilled water to avoid contamination |
| OTC Medications | May suppress cough or loosen mucus | Follow directions carefully, consult pharmacist if needed |
Medication Options for Treating Prednisone-Related Cough
Your doctor might prescribe medications to manage your prednisone-induced cough. These often address underlying causes or alleviate symptoms. Common choices include:
Addressing Underlying Causes
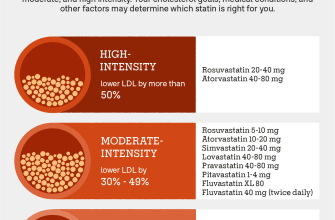
If your cough stems from irritation or inflammation in your lungs or airways (bronchitis, for example), your physician may prescribe bronchodilators like albuterol to relax airways and reduce coughing. For inflammation, inhaled corticosteroids, such as fluticasone, can be helpful. If a bacterial infection is suspected, antibiotics may be necessary.
Managing Symptoms
To relieve the cough itself, your doctor might suggest an antitussive medication like codeine or dextromethorphan, though these are generally used cautiously, especially given prednisone’s interactions. If the cough is accompanied by mucus, expectorants such as guaifenesin could help thin secretions and facilitate easier coughing. Remember to always discuss these options with your physician to assess potential interactions with prednisone and to find the best approach for your situation.
Preventing Prednisone-Induced Cough
Drink plenty of fluids, especially water, to thin mucus and ease coughing. Staying hydrated is key to reducing irritation in your airways.
Managing Underlying Conditions
Address any underlying respiratory conditions, like asthma or allergies, with your doctor. Effective management of these conditions minimizes the likelihood of prednisone exacerbating symptoms.
Use a humidifier to add moisture to the air, particularly in dry climates or during winter months. This soothes irritated airways and helps reduce coughing.
Consider a saline nasal spray to rinse nasal passages and remove irritants, which can indirectly alleviate coughing.
Avoid irritants such as smoke, dust, and strong fumes. These can worsen cough and make it harder to manage. Maintaining a clean environment at home and work is beneficial.
If your cough is severe or persistent, contact your physician immediately. They can assess your situation and adjust your treatment plan as needed.
Long-Term Effects and Considerations
Prolonged prednisone use can suppress your immune system, increasing susceptibility to infections. Monitor for any signs of infection and report them to your doctor immediately. This includes seemingly minor infections like colds or the flu.
Bone Health
Prednisone can weaken bones, increasing the risk of osteoporosis and fractures. Discuss bone density testing with your doctor and consider calcium and vitamin D supplements, along with weight-bearing exercise.
Glucose Metabolism
Prednisone can raise blood sugar levels, potentially worsening diabetes or causing it to develop. Regular blood glucose monitoring is recommended, especially if you have a history of diabetes or pre-diabetes. Your doctor may adjust your diabetes medication if needed.
Other Potential Side Effects
| Side Effect | Possible Solutions |
|---|---|
| Weight gain | Maintain a healthy diet and engage in regular exercise. |
| Mood changes | Open communication with your doctor and consider support groups. |
| High blood pressure | Regular blood pressure monitoring and potential medication adjustments. |
| Fluid retention | Dietary adjustments and close monitoring by your doctor. |
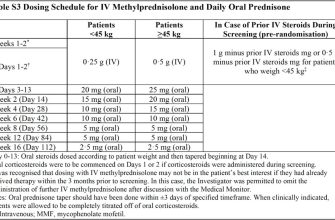
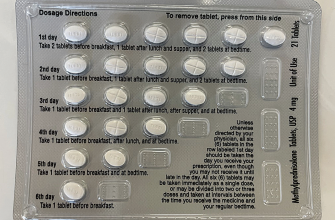
Tapering Off Prednisone
Never stop taking prednisone abruptly. Always follow your doctor’s instructions for gradually reducing the dosage to minimize withdrawal symptoms. This process can take several weeks or months, depending on your individual situation and the dosage.
Regular Monitoring
Schedule regular check-ups with your doctor to monitor your overall health and address any concerns that arise during prednisone treatment. Open communication with your healthcare provider is key to managing potential long-term effects.
Lifestyle Adjustments for Cough Relief During Prednisone Treatment
Hydrate consistently. Aim for at least eight glasses of water daily. This thins mucus, making it easier to cough up. Consider adding electrolyte drinks if you experience excessive sweating.
Humidify your environment. Dry air irritates the throat and worsens coughs. Use a humidifier or place bowls of water near radiators to add moisture to the air. Regularly clean your humidifier to prevent mold growth.
Managing Your Surroundings
Minimize exposure to irritants. Identify and avoid triggers such as smoke, dust, pollen, or strong fumes. This includes avoiding scented products and cleaning with mild, hypoallergenic detergents. Air purifiers can help filter out airborne particles.
Practice good sleep hygiene. Aim for 7-9 hours of sleep nightly in a cool, dark room. Rest allows your body to heal and reduces stress, which can exacerbate cough.
Dietary Considerations
Consume soothing foods and drinks. Warm broths, herbal teas (chamomile, ginger), and honey can coat and soothe your throat. Avoid caffeine and alcohol, which can dehydrate you.
Eat soft foods. Hard-to-chew foods can further irritate a sore throat. Opt for easily digestible options like oatmeal, yogurt, and mashed potatoes.
Other Strategies
Gargle with warm salt water. This can help reduce throat inflammation and loosen mucus. Mix 1/4 to 1/2 teaspoon of salt in 8 ounces of warm water and gargle several times a day.
Use throat lozenges or cough drops. Many are available over-the-counter and can provide temporary relief. Follow package directions carefully.
When to Seek Medical Attention
Contact your doctor if your cough persists or worsens despite these lifestyle changes, or if you experience shortness of breath, chest pain, or fever.