Generally, 5 mg of prednisone equals 20 mg of hydrocortisone. This conversion helps healthcare professionals and patients alike manage glucocorticoid therapies effectively. Remember, individual responses to these medications vary.
This ratio, however, isn’t a strict rule. Factors such as patient age, overall health, and the specific medical condition influence the appropriate dosage. Always consult your doctor for personalized medication guidance; they will consider your unique circumstances.
Never adjust your medication without consulting your physician. Incorrect dosage can have serious health implications. Your doctor will create a tailored treatment plan considering your needs and monitoring your progress.
This information is for educational purposes only and should not be considered medical advice. Always seek professional medical counsel for any health concerns or before making any decisions related to your health or treatment.
- Equivalent Prednisone to Hydrocortisone: A Practical Guide
- Understanding Prednisone and Hydrocortisone
- Conversion Charts: Prednisone to Hydrocortisone Equivalents
- Factors Influencing Dosage Conversion
- Calculating the Equivalent Dose for Different Administration Routes
- Intravenous and Intramuscular Conversions
- Important Note: Individual Variation
- Important Considerations for Medication Switching
- Dosage Conversion: A Careful Approach
- Monitoring Side Effects
- Timing and Administration
- Long-Term Implications
- Potential Side Effects and Monitoring
- Common Side Effects
- Less Common but Serious Side Effects
- Special Populations: Children and the Elderly
- Consulting Your Doctor: The Importance of Medical Supervision
- Managing Transition Between Medications
Equivalent Prednisone to Hydrocortisone: A Practical Guide
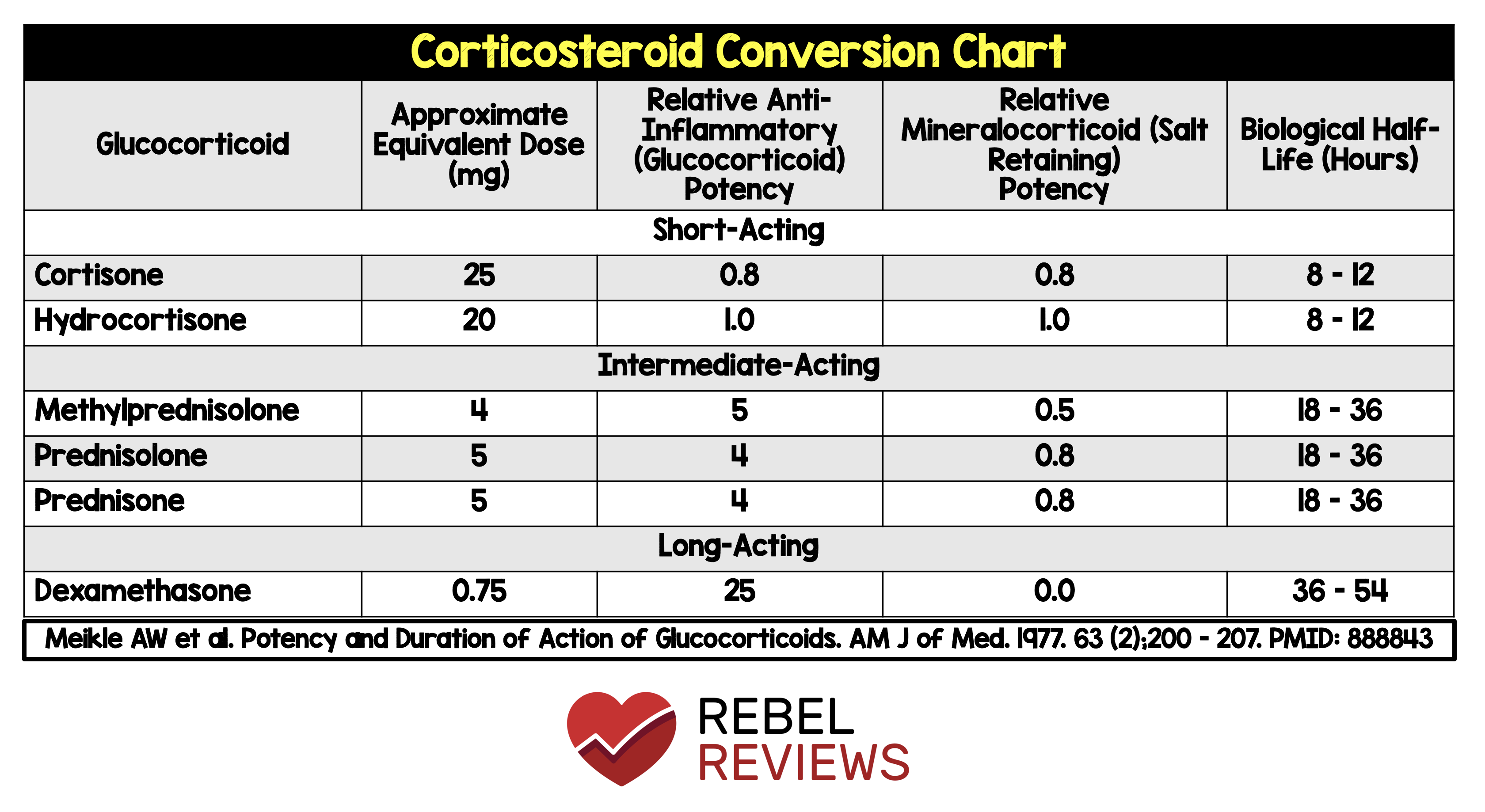
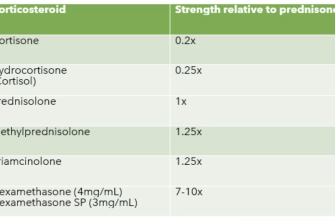
To convert between prednisone and hydrocortisone, remember that prednisone is approximately four times as potent as hydrocortisone. This means a smaller dose of prednisone will generally achieve the same effect as a larger dose of hydrocortisone.
Use the following conversion guideline as a starting point:
- Prednisone to Hydrocortisone: Multiply the prednisone dose by 4 to get an approximately equivalent hydrocortisone dose.
- Hydrocortisone to Prednisone: Divide the hydrocortisone dose by 4 to get an approximately equivalent prednisone dose.
For example:
- 20mg of prednisone is roughly equivalent to 80mg of hydrocortisone (20mg x 4 = 80mg).
- 100mg of hydrocortisone is roughly equivalent to 25mg of prednisone (100mg / 4 = 25mg).
Important Note: These are approximate conversions. Individual responses to medication vary. Your doctor should always supervise any dose adjustments, particularly during tapering or switching between these medications. Factors such as patient age, health status, and specific condition influence optimal dosage. Always discuss any medication changes with your physician. Don’t self-adjust your medication.
Here’s a table summarizing common conversion doses (remember, this is for guidance only and individual needs vary):
| Prednisone (mg) | Hydrocortisone (mg) |
|---|---|
| 5 | 20 |
| 10 | 40 |
| 20 | 80 |
| 30 | 120 |
| 40 | 160 |
This guide provides a general framework. Consult your healthcare provider for personalized advice and to ensure safe and effective medication management.
Understanding Prednisone and Hydrocortisone
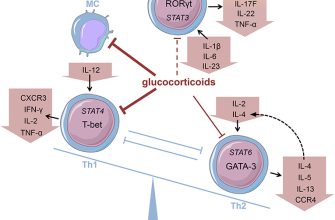
Prednisone and hydrocortisone are both corticosteroids, meaning they’re similar in structure and function. However, they differ in potency and how quickly your body metabolizes them.
Prednisone is a synthetic corticosteroid, meaning it’s not naturally found in the body. Your liver converts prednisone into prednisolone, the active form. This conversion takes time, leading to a delayed onset of action compared to hydrocortisone.
Hydrocortisone, on the other hand, is a natural corticosteroid also known as cortisol. Your body naturally produces it. Since it doesn’t require conversion, it offers a more immediate effect.
Dosage conversion between the two requires careful consideration. A general guideline often uses a 4:1 ratio (meaning 4mg of prednisone is approximately equivalent to 20mg of hydrocortisone), but this is only a rough estimate. Individual responses vary greatly, and a doctor should always determine the appropriate dose based on individual health needs and response.
Factors such as the specific condition being treated, the patient’s age, weight, and overall health significantly impact the conversion. Always consult your physician or pharmacist for precise dose adjustments; never attempt to self-adjust medication dosages.
Remember, both medications carry potential side effects. These can include increased blood sugar, weight gain, and changes in mood. Open communication with your healthcare provider about any concerns is vital for safe and effective treatment.
Conversion Charts: Prednisone to Hydrocortisone Equivalents
Use the following chart for approximate conversions. Remember that individual responses vary, and a doctor should always guide dosage adjustments.
Daily Dosage Conversion:
This chart provides a general guideline. Always consult your physician or pharmacist before making any changes to your medication.
| Prednisone (mg) | Hydrocortisone (mg) |
|---|---|
| 5 | 20 |
| 10 | 40 |
| 15 | 60 |
| 20 | 80 |
| 25 | 100 |
| 30 | 120 |
Important Considerations:
Route of administration significantly impacts conversion. Oral prednisone converts differently than intravenous hydrocortisone. The chart above refers to oral administration of both medications. Also, consider the patient’s medical history and current health status when making conversions. Dosage adjustments should be gradual to minimize adverse effects. Finally, regular monitoring of patient response is critical.
Disclaimer: This information is for educational purposes only and does not constitute medical advice. Always seek the guidance of a healthcare professional before changing medication dosages.
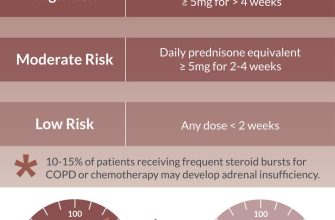
Factors Influencing Dosage Conversion
Accurate conversion requires careful consideration of several variables. Prednisone’s potency is approximately 4 times that of hydrocortisone. Therefore, a simple 4:1 ratio is a starting point, but this isn’t always accurate.
Patient-specific factors significantly impact conversion. Age, weight, and overall health status influence drug metabolism and response. For example, children often require higher doses per kilogram of body weight than adults.
The specific medical condition necessitates careful dosage adjustments. The severity of the condition and the desired therapeutic effect directly influence the appropriate dose. Conditions requiring immunosuppression may need higher doses compared to those requiring only anti-inflammatory action.
Route of administration matters. Oral prednisone and hydrocortisone are metabolized differently than intravenous or intramuscular forms. This affects bioavailability and therefore, the required dose.
Drug interactions can alter metabolism and efficacy. Concurrent medications may enhance or reduce the effect of both prednisone and hydrocortisone, affecting conversion calculations. Always check for potential drug interactions.
Finally, individual patient response varies. What works well for one person might not work for another. Close monitoring and dose titration are necessary to optimize treatment. Regular monitoring of blood tests and clinical symptoms guides dosage adjustments.
Calculating the Equivalent Dose for Different Administration Routes
Converting between prednisone and hydrocortisone dosages requires careful consideration of the administration route. A simple 1:1 ratio isn’t accurate. For oral administration, a commonly used conversion is 4mg of prednisone equivalent to 20mg of hydrocortisone. This means that a 20mg oral prednisone dose equates to a 100mg oral hydrocortisone dose. Remember, these are approximate conversions, and individual patient responses can vary.
Intravenous and Intramuscular Conversions
Intravenous (IV) and intramuscular (IM) administration often necessitates adjustments. For IV or IM routes, the equivalent dose may be slightly higher. A rough estimate is often to increase the oral equivalent dose by 20-30%. Therefore, a 100mg oral hydrocortisone dose might require 120-130mg IV or IM. Always consult prescribing information and medical literature for precise guidance based on the specific formulation and patient factors. This is not a substitute for professional medical advice.
Important Note: Individual Variation
Patient factors, including age, liver and kidney function, and concurrent medications significantly affect drug metabolism and response. These conversions serve as estimates only. A healthcare professional should always determine the appropriate dosage based on individual patient needs and monitoring response. Always discuss any dosage changes with your doctor or pharmacist.
Important Considerations for Medication Switching
Always consult your doctor before switching between prednisone and hydrocortisone. They will assess your individual needs and medical history to determine the appropriate dose and conversion strategy.
Dosage Conversion: A Careful Approach
Simple conversion ratios are unreliable. Prednisone and hydrocortisone have different potencies and metabolic pathways. A direct milligram-for-milligram exchange is inaccurate and potentially harmful.
- Typical Conversion: Rough estimates range from 3:1 to 5:1 (hydrocortisone:prednisone). But these are general guidelines, not precise formulas.
- Individual Variation: Your body’s response to corticosteroids varies. Factors like age, liver and kidney function, and other medications heavily influence the necessary dose.
- Gradual Adjustment: Your doctor will likely recommend a gradual taper or increase in dosage to minimize side effects and optimize therapeutic efficacy. Sudden changes can lead to serious health consequences.
Monitoring Side Effects
Closely monitor yourself for side effects during and after the medication switch. Report any changes to your doctor immediately.
- Increased Blood Sugar: Monitor blood glucose levels, especially if you have diabetes.
- Fluid Retention: Watch for swelling in your extremities.
- Mood Changes: Be aware of any unusual irritability, anxiety, or depression.
- Increased Blood Pressure: Regular blood pressure checks are crucial.
- Weakened Immune System: Take precautions to avoid infections.
Timing and Administration
The time of day you take your medication matters. Your doctor will provide specific instructions to maintain consistent blood levels.
- Morning Dosing: Frequently prescribed to mimic the body’s natural cortisol rhythm.
- Specific Instructions: Follow your doctor’s instructions precisely regarding timing and method of administration (oral, intravenous, etc.).
Long-Term Implications
Long-term use of corticosteroids carries risks. Discuss long-term management strategies with your doctor, including potential weaning off the medication.
Potential Side Effects and Monitoring
Both prednisone and hydrocortisone can cause side effects, varying in severity depending on dosage and duration of treatment. Close monitoring is key.
Common Side Effects
- Increased blood sugar: Monitor blood glucose regularly, especially if you have diabetes. Adjust medication as needed, in consultation with your doctor.
- Weight gain: Maintain a healthy diet and exercise routine. Discuss weight management strategies with your healthcare provider.
- Fluid retention: Observe for swelling in your ankles, feet, or face. Report any significant swelling to your doctor.
- Mood changes: Be mindful of irritability, anxiety, or depression. Seek support if needed.
- Insomnia: Avoid caffeine and alcohol before bed. Establish a regular sleep schedule.
- Increased appetite: Make conscious choices to maintain a balanced diet. Portion control can help.
- High blood pressure: Regular blood pressure checks are vital. Follow your doctor’s advice for managing blood pressure.
Less Common but Serious Side Effects
- Osteoporosis: Discuss bone density testing with your doctor, especially with prolonged use. Calcium and vitamin D supplements might be recommended.
- Increased risk of infection: Practice good hygiene and report any signs of infection immediately.
- Cushing’s syndrome: This rare but serious condition involves the body producing too much cortisol. Regular check-ups with your doctor are crucial.
- Gastrointestinal issues: Take medication with food to minimize stomach upset. Report persistent nausea or vomiting.
Regular check-ups with your physician are crucial for monitoring your health and adjusting medication accordingly. Open communication with your doctor is vital for managing potential side effects and ensuring optimal treatment.
Special Populations: Children and the Elderly
Children require lower doses of hydrocortisone compared to prednisone, often calculated based on body weight. A common pediatric conversion is 4 mg of prednisone to 5 mg of hydrocortisone per kilogram of body weight. Close monitoring for side effects, such as growth suppression, is crucial. Always consult a pediatric endocrinologist for precise dosage adjustments.
Elderly patients, conversely, may be more sensitive to both medications. Start with lower doses and monitor closely for adverse effects such as osteoporosis, increased risk of infections, and cardiovascular complications. Regular bone density testing might be advisable, and dose reductions should be gradual to minimize withdrawal symptoms. Careful consideration of concomitant medications is necessary to avoid drug interactions.
Consulting Your Doctor: The Importance of Medical Supervision
Never adjust your prednisone or hydrocortisone dosage without your doctor’s explicit guidance. These medications have significant side effects, and incorrect dosing can be harmful.
Regular check-ups allow your doctor to monitor your progress, adjust your medication as needed, and address any potential complications. This includes blood pressure, blood sugar, and bone density checks – all potentially affected by corticosteroid use.
Open communication is key. Report any new symptoms or changes in your health immediately. This might include weight gain, mood swings, increased thirst, or frequent infections. Early detection allows for prompt intervention.
Your doctor can help you create a tapering schedule for safely reducing your corticosteroid dose. Stopping abruptly can lead to serious withdrawal symptoms. A gradual reduction minimizes these risks.
| Symptom | Action |
|---|---|
| Increased thirst | Contact your doctor immediately. This might indicate high blood sugar. |
| Unexplained weight gain | Discuss this with your doctor; they may adjust your medication or recommend lifestyle changes. |
| Frequent infections | Report these promptly. Your immune system may be suppressed. |
| Mood changes | Let your doctor know. They can offer support and potentially adjust your medication. |
Remember, your doctor is your partner in managing your health. Their expertise ensures safe and effective treatment. Active participation in your care ensures the best possible outcome.
Managing Transition Between Medications
Your doctor will carefully plan your switch from prednisone to hydrocortisone, or vice versa. This often involves a gradual reduction of one medication while slowly increasing the other. This tapering process minimizes the risk of withdrawal symptoms and helps your body adjust.
Closely monitor your symptoms throughout the transition. Report any new or worsening symptoms to your physician immediately. This proactive approach is key to a smooth transition.
Accurate dosing is paramount. Use a reliable measuring device, such as a calibrated oral syringe, to ensure precise medication administration. Improper dosing can lead to complications.
Maintaining regular communication with your healthcare provider is vital. Schedule follow-up appointments as recommended to discuss your progress, adjust dosages if needed, and address any concerns. This ensures optimal medication management.
| Medication | Typical Dosage Adjustment Strategy | Important Considerations |
|---|---|---|
| Prednisone to Hydrocortisone | A slow decrease in prednisone while gradually increasing hydrocortisone, with careful monitoring of symptoms. | Pay close attention to cortisol levels. Hydrocortisone replacement needs to adequately address your body’s cortisol production deficiency. |
| Hydrocortisone to Prednisone | A gradual decrease in hydrocortisone while carefully introducing prednisone. The rate of reduction depends on individual factors. | Monitor for adrenal suppression. Prednisone is generally more potent and requires careful dosage management. |
Remember, every individual responds differently to medication changes. Your doctor will personalize the transition based on your specific medical history, current health status, and response to treatment. Follow their instructions closely.