High-dose prednisone offers a potent anti-inflammatory effect, often used in MS to manage acute exacerbations. Expect rapid symptom improvement within days for many, but understand that it’s a short-term solution, not a long-term disease modifier. This means that the effects are usually temporary and don’t affect the disease progression.
Typical treatment involves a daily dose of 1000mg, tapered down over several weeks to minimize withdrawal effects. Close monitoring of blood sugar and blood pressure is paramount due to the potential side effects of high-dose steroids. Discuss potential interactions with any other medications you are taking with your doctor before starting treatment.
Remember that side effects are common and can include weight gain, insomnia, mood swings, increased appetite, and increased risk of infection. Your physician will carefully weigh the benefits against the risks, considering your specific circumstances and medical history. Open communication with your healthcare provider is crucial throughout the treatment process to manage any side effects that arise and adjust the dosage as needed.
Always consult with your neurologist or MS specialist before starting any treatment, including high-dose prednisone. They can help you assess your individual needs and develop a tailored treatment plan.
- High Dose Prednisone in Multiple Sclerosis: A Detailed Overview
- Potential Benefits
- Potential Risks and Side Effects
- Monitoring and Management
- Alternative and Complementary Treatments
- Prednisone Dosage and Tapering Schedule Example
- Long-Term Implications
- What is High-Dose Prednisone and How Does it Work in MS?
- Short-Term Benefits and Risks of High-Dose Prednisone for MS Relapses
- Benefits:
- Risks:
- Long-Term Effects and Side Effects of High-Dose Prednisone Use
- Who is a Candidate for High-Dose Prednisone Treatment?
- Determining Suitability
- Who Might Not Be a Candidate?
- Next Steps
- Alternative Treatments and When They Might Be Preferred Over Prednisone
- Managing Side Effects of High-Dose Prednisone: Practical Tips
- Monitoring and Follow-up After High-Dose Prednisone Treatment
High Dose Prednisone in Multiple Sclerosis: A Detailed Overview
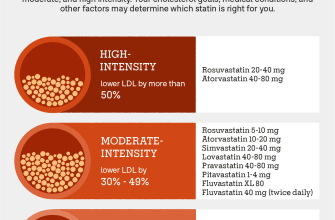
High-dose prednisone is a common treatment for MS relapses, aiming to reduce inflammation and improve symptoms quickly. A typical course involves a daily dose of 1000mg for three days, tapering down over several weeks. This aggressive approach isn’t without risks, however, so careful monitoring is crucial.
Potential Benefits
High-dose prednisone can significantly reduce the duration and severity of MS relapses. Many patients experience improvements in vision, mobility, and other neurological symptoms within days of starting treatment. This rapid response offers significant relief during acute attacks.
Potential Risks and Side Effects
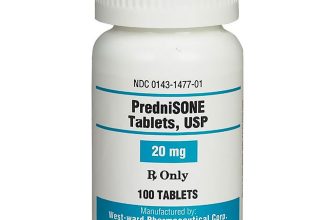
The significant side effects of high-dose prednisone must be carefully considered. Common short-term effects include increased appetite, weight gain, mood swings, insomnia, and increased blood sugar levels. Long-term use increases the risk of osteoporosis, cataracts, and cardiovascular problems. Serious side effects, though rare, include infections and increased risk of bleeding.
Monitoring and Management
Regular monitoring is vital throughout the treatment and tapering process. Doctors closely track blood pressure, blood sugar, and bone density. Lifestyle adjustments, such as a healthy diet and regular exercise, can help mitigate some side effects. Close communication with your physician is paramount.
Alternative and Complementary Treatments
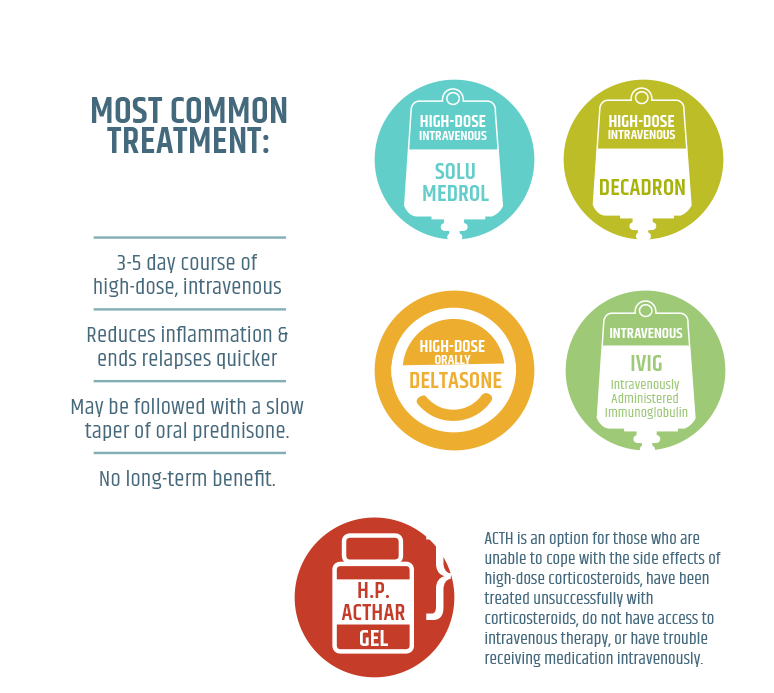
High-dose prednisone isn’t always the first choice. Disease-modifying therapies (DMTs) aim to slow disease progression, but they work more slowly. Other therapies, such as plasma exchange or intravenous immunoglobulin (IVIG), are considered in certain cases. The choice of treatment depends on the individual patient and their specific situation.
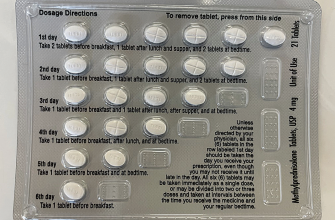
Prednisone Dosage and Tapering Schedule Example
| Day | Dose (mg) |
|---|---|
| 1-3 | 1000 |
| 4-7 | 750 |
| 8-11 | 500 |
| 12-15 | 250 |
| 16-21 | 125 |
| 22-28 | 62.5 |
| 29+ | 0 |
Note: This is a sample tapering schedule. Your doctor will create a personalized plan based on your individual needs and response to treatment.
Long-Term Implications
While offering short-term relief, high-dose prednisone shouldn’t be considered a long-term solution for MS management. Its use is generally limited to managing relapses. Long-term use necessitates careful consideration of the cumulative risks and benefits.
What is High-Dose Prednisone and How Does it Work in MS?
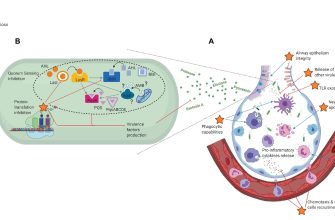
High-dose prednisone is a powerful corticosteroid, typically administered orally in doses exceeding 40mg daily, sometimes reaching much higher levels depending on the severity of the MS attack. It doesn’t cure MS, but it significantly reduces inflammation in the central nervous system.
Prednisone works by suppressing the immune system. This dampens the inflammatory response responsible for MS attacks, thus reducing symptoms such as numbness, weakness, and vision problems. The effects are usually noticed within days. The specific mechanism involves several pathways, including decreasing the production of inflammatory cytokines and reducing the infiltration of immune cells into the brain and spinal cord.
Doctors often prescribe a “pulse” of high-dose prednisone for short periods, followed by a gradual tapering of the dosage to minimize side effects. This approach targets the acute inflammation during an MS relapse. Long-term use of high-dose prednisone is generally avoided due to significant risks.
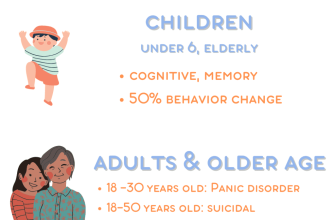
Common side effects include weight gain, increased appetite, mood swings, insomnia, increased blood sugar, and increased risk of infections. Your doctor will carefully monitor these and adjust the treatment plan accordingly. Always discuss any concerns or side effects you experience with your medical team.
Remember, high-dose prednisone is a treatment for MS relapses, not a long-term solution. It’s a powerful tool used strategically as part of a broader MS management plan, usually in conjunction with other disease-modifying therapies.
Short-Term Benefits and Risks of High-Dose Prednisone for MS Relapses
High-dose prednisone, typically administered as a short course (e.g., 1-2 weeks), offers rapid symptom improvement for many experiencing MS relapses. This quick reduction in inflammation helps lessen neurological deficits like weakness, numbness, and vision problems.
Benefits:
- Faster symptom relief: Many patients report noticeable improvement within days of starting treatment.
- Reduced inflammation: Prednisone powerfully suppresses the immune system, directly addressing the inflammatory process driving MS relapses.
- Improved quality of life: Faster symptom relief translates to improved daily functioning and overall well-being during the acute phase of a relapse.
Risks:
- Side effects: High-dose prednisone carries significant side effects, including increased blood sugar, weight gain, insomnia, mood swings, and increased risk of infections. These effects are often temporary, but their severity varies between individuals.
- Increased relapse frequency: While prednisone manages the current relapse, some research suggests it might increase the likelihood of future relapses, though this is a topic of ongoing research and isn’t uniformly observed.
- Bone loss (osteoporosis): Long-term use of corticosteroids is linked to bone thinning. While a short course minimizes this risk, it’s still a factor to consider, particularly for individuals already at risk for osteoporosis.
- Medication interactions: Prednisone can interact with other medications, including some commonly used for MS. Consult your neurologist to ensure no adverse interactions occur.
Your doctor will carefully weigh the potential benefits against the risks before prescribing high-dose prednisone. Factors considered include the severity of your relapse, your overall health, and your response to other treatments. Open communication with your neurologist is crucial throughout this process.
- Regular monitoring: Close monitoring for side effects during and after treatment is essential.
- Tapering schedule: Prednisone should always be tapered gradually to reduce the risk of withdrawal symptoms and adrenal suppression.
- Lifestyle adjustments: A healthy diet, exercise, and sufficient sleep can help mitigate some of the side effects.
Remember that high-dose prednisone is a short-term solution for managing MS relapses, not a long-term disease-modifying therapy. Discuss long-term disease management strategies with your neurologist to effectively manage your MS and prevent future relapses.
Long-Term Effects and Side Effects of High-Dose Prednisone Use
High-dose prednisone, while effective for managing MS relapses, carries significant risks with prolonged use. Expect potential weight gain, often significant and difficult to manage. Increased appetite accompanies this, potentially leading to further weight problems.
Osteoporosis is a serious concern. Prednisone weakens bones, increasing fracture risk. Regular bone density checks and potentially medication to protect bone health are recommended.
Increased blood sugar levels are common, raising the risk of type 2 diabetes. Monitor blood sugar regularly, especially if you have a family history of diabetes. Dietary changes and medication may be necessary.
High blood pressure is another prevalent side effect. Regular monitoring and lifestyle adjustments, including diet and exercise, are crucial. Your doctor might prescribe medication to control blood pressure.
Prednisone can cause mood swings, including irritability, anxiety, and even depression. Open communication with your doctor is vital for managing these mental health effects. Therapy or medication may be helpful.
Cataracts and glaucoma are potential long-term eye problems. Regular eye exams are strongly advised to detect and treat these conditions early.
Muscle weakness and thinning of the skin are other possible side effects. Regular exercise, a balanced diet, and potentially supplemental protein can help mitigate muscle loss. Skin care routines should focus on hydration and sun protection.
Infections become more likely with long-term prednisone use, due to its immunosuppressant effects. Practice good hygiene and seek medical attention for any signs of infection.
Withdrawal from high-dose prednisone must be gradual to avoid potentially serious complications. Your doctor will create a tapering schedule to minimize adverse effects during the withdrawal process.
Remember, these are potential side effects; not everyone experiences them all, or even any of them. The severity and presence of these side effects vary depending on the dose, duration of treatment, and individual factors. Consistent communication with your neurologist is key to managing the risks and benefits of high-dose prednisone treatment for your MS.
Who is a Candidate for High-Dose Prednisone Treatment?
High-dose prednisone is typically considered for individuals experiencing a severe MS relapse, characterized by significant neurological dysfunction. This means symptoms like significant vision loss, severe weakness affecting mobility, or substantial speech or cognitive impairment. Your neurologist will assess the severity and impact of your relapse on your daily life.
Determining Suitability
Doctors consider several factors before prescribing high-dose prednisone. The specific symptoms, their duration and intensity, and your overall health are key. A recent MRI scan showing active lesions may also support this treatment option. However, the presence of active lesions alone doesn’t automatically qualify someone for high-dose prednisone. The decision rests on a holistic assessment of your condition.
Who Might Not Be a Candidate?
Certain conditions can rule out high-dose prednisone. Pre-existing health issues like diabetes, hypertension, infections, or peptic ulcers require careful consideration. The risks associated with high-dose steroids might outweigh the benefits in these cases. Your doctor will thoroughly review your medical history to minimize potential complications.
Next Steps
Remember: High-dose prednisone is not a long-term solution for MS. It’s primarily used to manage acute relapses and reduce inflammation. Your neurologist will discuss appropriate disease-modifying therapies for long-term management after your relapse subsides. Open communication with your doctor is critical for determining the best course of treatment for your specific needs.
Alternative Treatments and When They Might Be Preferred Over Prednisone
Consider disease-modifying therapies (DMTs) like interferon beta, glatiramer acetate, or natalizumab. These medications aim to slow MS progression, unlike prednisone, which primarily manages acute relapses. Choose DMTs if you need long-term management and want to reduce relapse frequency.
B-cell depleting therapies, such as rituximab or ocrelizumab, offer another avenue. They target specific immune cells contributing to MS. Opt for these if interferon or glatiramer acetate prove insufficient, or if you experience frequent relapses despite these treatments.
For those with severe, rapidly progressing MS, consider alemtuzumab or other highly effective DMTs. These therapies offer stronger immunosuppression, suitable for cases where other treatments have failed to provide adequate control. Remember to discuss risks and benefits thoroughly with your neurologist.
Physical therapy, occupational therapy, and speech therapy can significantly improve quality of life, regardless of medication choices. These therapies address physical limitations caused by MS, helping maintain mobility, independence, and communication skills. Integrate these therapies into your overall treatment plan.
Lifestyle modifications, including regular exercise, stress management techniques, and a healthy diet, provide additional support. These changes positively impact overall health and well-being, potentially reducing symptom severity and improving disease management. Consult a healthcare professional to develop a personalized plan.
Your neurologist will help you determine the best treatment approach based on your specific MS type, disease activity, and individual needs. Open communication with your doctor is key to making informed decisions about your care.
Managing Side Effects of High-Dose Prednisone: Practical Tips
Eat smaller, frequent meals throughout the day to manage nausea and stomach upset. This prevents overwhelming your digestive system.
Increase your potassium intake with foods like bananas, potatoes, and leafy greens. Prednisone can lower potassium levels.
Drink plenty of water to stay hydrated, counteracting fluid retention and potential constipation.
Monitor your blood sugar regularly, especially if you have diabetes or risk factors. Prednisone can elevate blood sugar.
Maintain a healthy diet low in processed foods and refined sugars to mitigate weight gain and other metabolic side effects.
Consider regular, gentle exercise like walking to combat fatigue and improve mood. Always consult your doctor before starting any new exercise program.
Use mild soap and lukewarm water when showering to minimize skin thinning and dryness. Avoid harsh chemicals and hot water.
Discuss sleep disturbances with your doctor; they may prescribe medication to help regulate your sleep cycle.
Report any vision changes or increased eye pressure to your ophthalmologist immediately. Prednisone can impact eye health.
Keep a journal to track side effects and their severity. This helps you and your doctor monitor treatment and adjust accordingly.
Communicate openly with your doctor about any concerns or worsening symptoms. They can provide personalized guidance and adjust your treatment plan as needed.
Monitoring and Follow-up After High-Dose Prednisone Treatment
Regular monitoring is crucial after high-dose prednisone. Your doctor will schedule appointments to track your progress and manage potential side effects.
- Blood pressure: Expect frequent blood pressure checks, as prednisone can elevate it. Medication adjustments may be necessary.
- Blood sugar: High-dose prednisone frequently impacts blood sugar levels. Regular blood glucose monitoring is vital, particularly if you have diabetes or risk factors.
- Weight: Prednisone can cause weight gain. Monitor your weight and discuss dietary adjustments with your doctor or a registered dietitian.
- Bone density: Long-term high-dose prednisone weakens bones. Your doctor might recommend bone density scans to assess risk and suggest preventative measures, like calcium and vitamin D supplements.
- Mood changes: Prednisone can affect mood, leading to anxiety, depression, or irritability. Openly communicate any emotional shifts to your healthcare provider. They may prescribe mood stabilizers or refer you to a mental health professional.
Beyond routine blood tests, your neurologist will assess your MS symptoms. They’ll evaluate your relapse frequency, disease activity, and overall neurological function. MRI scans may be used to monitor disease progression.
- Tapering Schedule: Expect a gradual reduction in prednisone dosage, not a sudden stop. This minimizes withdrawal symptoms like fatigue and joint pain.
- Symptom Management: Your doctor will work with you to manage side effects, potentially prescribing additional medications to alleviate specific issues.
- Disease-Modifying Therapies (DMTs): High-dose prednisone is not a long-term solution for MS. Discuss appropriate DMTs with your neurologist to manage your disease long-term.
Maintain open communication with your healthcare team. Report any concerning changes or unexpected side effects immediately. Proactive monitoring and collaboration ensure the best possible outcome from your high-dose prednisone treatment and subsequent management of your MS.