Never combine levofloxacin and prednisone without explicit physician guidance. This combination carries potential risks, primarily the increased chance of tendon rupture, especially in older adults or those with kidney issues. Your doctor will weigh the benefits against these risks before prescribing both medications simultaneously.
If prescribed this combination, meticulously follow dosage instructions. Consistent medication adherence is critical to treatment success and minimizing adverse effects. Report any new or worsening symptoms, such as tendon pain or swelling, muscle weakness, or unusual bruising, immediately to your doctor. Prompt attention to these signs is paramount.
Consider keeping a detailed record of your medication intake, including any side effects you experience. This information will be incredibly helpful during follow-up appointments. Your doctor can then adjust the treatment plan as needed, based on your individual response to the medication. Regular blood tests may also be required to monitor potential drug interactions.
Remember, this information serves as a general guide only. Always consult your healthcare provider for personalized advice tailored to your specific medical history and current health status. Self-treating can be dangerous; professional medical guidance is always necessary.
- Levofloxacin and Prednisone: A Detailed Overview
- Potential Side Effects and Interactions
- Dosage and Administration
- Understanding Levofloxacin’s Role in Infection Treatment
- Prednisone’s Mechanism of Action in Inflammation Reduction
- Impact on Immune Cells
- Stabilization of Lysosomal Membranes
- Combined Use: When is Levofloxacin and Prednisone Prescribed Together?
- Potential Drug Interactions and Side Effects
- Gastrointestinal Effects
- Other Potential Interactions
- Monitoring and Reporting
- Patient Considerations: Monitoring and Precautions
- Monitoring Blood Sugar
- Medication Interactions
- Sun Sensitivity
- Alternatives and Future Directions in Treatment
- Non-Antibiotic Approaches
- Personalized Medicine
- Future Research
Levofloxacin and Prednisone: A Detailed Overview
Combining levofloxacin and prednisone requires careful monitoring. Levofloxacin, a fluoroquinolone antibiotic, treats bacterial infections. Prednisone, a corticosteroid, reduces inflammation. Their interaction can increase the risk of tendon rupture, especially in older adults or those with pre-existing conditions like kidney or liver problems. Closely monitor for tendon pain or inflammation. Report any unusual symptoms to your doctor immediately.
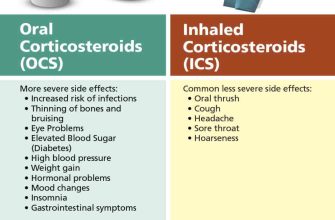
Potential Side Effects and Interactions
Combining these medications might increase the risk of side effects from both drugs. Prednisone can raise blood sugar levels, while levofloxacin can impact the heart’s rhythm. You might experience gastrointestinal upset, such as nausea or diarrhea, from either drug. Furthermore, levofloxacin can interact with medications metabolized by the liver, potentially altering their effectiveness. Always inform your physician about all medications, supplements, and herbal remedies you’re taking.
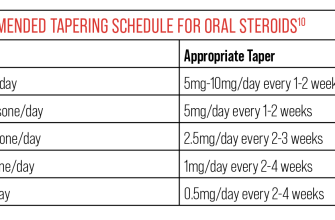
Dosage and Administration
Your doctor will determine the appropriate dosage of each medication based on your individual health needs and the specific infection being treated. Never adjust your dosage without consulting your physician. Follow prescribed instructions carefully. Prednisone is often used for a limited duration, while levofloxacin treatment depends on the infection’s severity.
Understanding Levofloxacin’s Role in Infection Treatment
Levofloxacin combats bacterial infections by interfering with their DNA replication. This prevents bacteria from multiplying and allows the body’s immune system to clear the infection. It’s a fluoroquinolone antibiotic, effective against a broad spectrum of gram-positive and gram-negative bacteria.
Doctors prescribe levofloxacin for various infections, including:
| Infection Type | Specific Examples |
|---|---|
| Respiratory Tract Infections | Pneumonia, bronchitis, sinusitis |
| Skin and Soft Tissue Infections | Cellulitis, abscesses |
| Urinary Tract Infections | Cystitis, pyelonephritis |
| Anthrax | Inhalation anthrax (prophylaxis and treatment) |
Remember, levofloxacin is a powerful medication. Always follow your doctor’s instructions regarding dosage and duration of treatment. Failure to complete the prescribed course can lead to treatment failure and the development of antibiotic-resistant bacteria. Report any side effects immediately to your healthcare provider.
Specific dosages vary based on the infection and individual patient factors. Your doctor will determine the appropriate dose and length of treatment for your particular situation. They will also assess potential drug interactions and consider your medical history before prescribing levofloxacin.
While generally safe, levofloxacin can have side effects, such as nausea, diarrhea, headache, and dizziness. Serious, though rare, side effects may include tendon rupture and peripheral neuropathy. Discuss potential risks and benefits thoroughly with your doctor before starting treatment.
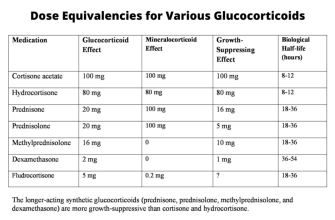
Prednisone’s Mechanism of Action in Inflammation Reduction
Prednisone, a glucocorticoid, potently reduces inflammation by binding to intracellular glucocorticoid receptors. This binding initiates a cascade of events impacting gene transcription. Specifically, it inhibits the production of inflammatory mediators like cytokines (e.g., TNF-α, IL-1, IL-6) and prostaglandins.
Impact on Immune Cells
Prednisone also directly affects immune cells. It reduces the activity of lymphocytes, monocytes, and macrophages, thereby decreasing the inflammatory response. This action involves suppressing the proliferation and activation of these cells.
Stabilization of Lysosomal Membranes
Furthermore, prednisone stabilizes lysosomal membranes. This prevents the release of destructive enzymes that contribute to tissue damage in inflammatory processes. The net result is a reduction in tissue swelling, pain, and redness.
Combined Use: When is Levofloxacin and Prednisone Prescribed Together?
Doctors often prescribe levofloxacin and prednisone together to treat severe bacterial infections, particularly those involving inflammation. This combination targets both the infection itself and the associated inflammatory response.
Respiratory infections like pneumonia or bronchitis are common reasons for this combined prescription. Levofloxacin, a fluoroquinolone antibiotic, directly combats the bacteria causing the infection. Prednisone, a corticosteroid, reduces swelling and inflammation in the airways, improving breathing and overall comfort.
Infections of the skin and soft tissues also sometimes warrant this dual approach. Prednisone helps manage the significant inflammation often accompanying these infections, while levofloxacin eradicates the causative bacteria. Careful monitoring is necessary due to the risk of side effects.
In some cases, severe exacerbations of chronic obstructive pulmonary disease (COPD) may require this combined therapy. Prednisone helps manage the acute airway inflammation, while levofloxacin addresses potential bacterial involvement.
It’s crucial to remember this is not a standard treatment for every infection. Your doctor will consider various factors, such as the specific infection, its severity, your medical history, and possible drug interactions, before prescribing this combination. Always discuss potential risks and benefits with your healthcare provider.
Potential Drug Interactions and Side Effects
Combining levofloxacin and prednisone requires careful monitoring. Levofloxacin, a fluoroquinolone antibiotic, can increase the risk of tendon rupture, a side effect amplified by prednisone, a corticosteroid. This risk is particularly high in older adults and those with kidney problems. Therefore, you should immediately report any tendon pain or inflammation to your doctor.
Gastrointestinal Effects
Both medications can cause gastrointestinal upset. Prednisone may lead to increased stomach acid production, increasing the likelihood of ulcers. Levofloxacin frequently causes nausea, diarrhea, and vomiting. Consider taking these medications with food to minimize stomach irritation. If you experience severe or persistent gastrointestinal issues, contact your healthcare provider.
Other Potential Interactions
Levofloxacin interacts with various medications, including antacids containing magnesium or aluminum, which can reduce its absorption. Prednisone’s interaction profile is extensive; it can affect blood sugar levels, impacting the effectiveness of diabetes medications. Always provide your doctor with a complete list of all your medications and supplements to avoid dangerous interactions. Regular blood tests may be necessary to monitor for side effects and drug levels.
Monitoring and Reporting
Closely monitor yourself for any unusual symptoms, such as changes in vision, mental status alterations, or severe allergic reactions. Report any new or worsening symptoms immediately. Your doctor should regularly assess your progress and adjust the medication regimen as needed based on your individual response and overall health. Open communication with your healthcare provider is key to safe and effective treatment.
Patient Considerations: Monitoring and Precautions
Regularly monitor for signs of Clostridium difficile infection (CDI), such as diarrhea. Report any significant changes in bowel habits to your doctor immediately. This is particularly important given the potential link between fluoroquinolones like levofloxacin and CDI.
Keep your doctor informed about any new or worsening symptoms, including tendon pain, especially in the Achilles tendon. Levofloxacin can increase the risk of tendon rupture. Rest is crucial if you experience any tendon pain.
Monitoring Blood Sugar
If you have diabetes, closely monitor your blood sugar levels. Prednisone can elevate blood glucose. Adjust your diabetes medication as needed, following your doctor’s instructions. Frequent blood sugar checks are recommended while on this medication combination.
Medication Interactions
Disclose all medications, including over-the-counter drugs and supplements, to your doctor or pharmacist. Some medications can interact negatively with levofloxacin or prednisone. This includes antacids, which can reduce levofloxacin absorption. Accurate and complete information ensures optimal treatment safety.
Sun Sensitivity
Prednisone can increase your sensitivity to sunlight. Use sunscreen with a high SPF and wear protective clothing when outdoors. Avoid prolonged sun exposure to minimize the risk of sunburn. This precaution is especially important during peak sun hours.
Alternatives and Future Directions in Treatment
For bacterial infections requiring broad-spectrum coverage, consider azithromycin or a combination of amoxicillin and clavulanate as alternatives to levofloxacin. These options often provide comparable efficacy with a lower risk of adverse effects, particularly concerning antibiotic resistance.
Non-Antibiotic Approaches
For inflammatory components, consider targeted therapies like selective COX-2 inhibitors (e.g., celecoxib) instead of prednisone, minimizing systemic corticosteroid side effects. These offer anti-inflammatory benefits with a potentially reduced risk of immunosuppression.
- Biologics: In specific cases, biologics like anti-TNF agents might offer targeted therapy for inflammation, but this decision requires careful consideration by specialists due to potential risks and high cost.
- Immunomodulators: Depending on the underlying condition, immunomodulatory drugs might be explored as an alternative to prednisone, offering a different approach to inflammatory control.
Personalized Medicine
Future treatment strategies will likely integrate personalized medicine. This involves tailoring treatment to the individual’s genetic makeup, microbiome, and specific infection characteristics. Genetic testing could help predict treatment response and minimize adverse effects.
- Pharmacogenomics: This field examines how genes affect drug response, allowing for personalized antibiotic selection and dosage adjustments.
- Microbiome analysis: Studying the gut microbiome’s composition may identify specific microbial targets for treatment, further guiding personalized therapy choices.
Future Research
Ongoing research focuses on developing novel antibiotics with targeted mechanisms of action and reduced resistance profiles. Furthermore, exploring advanced drug delivery systems promises improved efficacy and reduced side effects. This includes targeted delivery of antibiotics directly to the infection site.