Consider low-dose prednisone (less than 20mg daily) as a short-term treatment option for severe psoriasis flare-ups, under strict dermatological supervision. This approach aims to quickly reduce inflammation and alleviate symptoms, improving quality of life while minimizing potential side effects associated with higher dosages.
Your doctor will carefully assess your specific condition, including the severity and location of your psoriasis, before prescribing low-dose prednisone. They’ll likely recommend a gradual tapering schedule to reduce the risk of withdrawal symptoms and prevent relapse. Remember, this isn’t a long-term solution; expect treatment duration to be measured in weeks, not months. Regular blood tests may be necessary to monitor potential side effects.
Combining low-dose prednisone with other treatments, such as topical corticosteroids or biologics, is frequently a more effective strategy for long-term psoriasis management. This multi-pronged approach often leads to better control and reduced reliance on systemic medications like prednisone. Discuss this comprehensive strategy with your dermatologist to find the best treatment plan tailored for your needs.
Important Note: Never adjust your prednisone dosage without consulting your doctor. Sudden cessation can trigger serious health complications. Open communication with your healthcare provider is crucial for optimal outcomes and minimizing potential risks.
- Low Dose Prednisone for Psoriasis: A Detailed Overview
- What is Psoriasis and How Does Prednisone Work?
- Low-Dose Prednisone: Dosage and Administration
- Benefits and Potential Side Effects of Low-Dose Prednisone
- Potential Benefits
- Potential Side Effects
- Important Note:
- When is Low-Dose Prednisone Appropriate for Psoriasis?
- Combining Low-Dose Prednisone with Other Treatments
- Monitoring Progress and Adjusting Treatment
- Long-Term Use and Potential Risks
- Monitoring Your Health
- Alternative Treatments
- Alternative Treatments and Lifestyle Changes
- Dietary Adjustments
- Stress Management Techniques
- Topical Treatments
- Skincare Routine
- Exercise and Sleep
- Biologics and Other Medications
Low Dose Prednisone for Psoriasis: A Detailed Overview
Prednisone, a corticosteroid, offers short-term relief from psoriasis symptoms at low doses. However, it’s crucial to understand its limitations and potential side effects.
Low-dose prednisone typically involves daily dosages ranging from 5 to 20mg. Your dermatologist determines the appropriate dose based on your individual needs and the severity of your psoriasis. Higher doses are generally avoided due to increased side effect risks.
- Benefits: Low-dose prednisone quickly reduces inflammation and lessens the severity of psoriasis plaques, providing noticeable symptom relief. This can be especially helpful during flare-ups.
- Limitations: Prednisone only treats symptoms; it doesn’t cure psoriasis. Stopping the medication usually leads to a return of symptoms. Long-term use carries significant risks.
Potential side effects, even at low doses, include:
- Increased appetite and weight gain
- Mood changes, including irritability or anxiety
- Insomnia
- Increased blood sugar levels
- High blood pressure
- Thinning of the skin
Low-dose prednisone is often part of a broader treatment plan. Doctors frequently combine it with other psoriasis therapies such as topical medications, phototherapy, or biologics. This approach maximizes benefits while minimizing prednisone’s duration and thus, potential side effects.
- Discuss Treatment Options: Always consult your dermatologist. They will assess your psoriasis and create a personalized treatment plan.
- Monitor Side Effects: Closely monitor your body for any adverse reactions. Report any concerning symptoms to your doctor immediately.
- Gradual Tapering: Never stop prednisone abruptly. Your doctor will gradually reduce your dose to minimize withdrawal symptoms.
- Lifestyle Changes: Maintain a healthy lifestyle, including a balanced diet, regular exercise, and stress management techniques, to support your overall health and manage psoriasis.
Remember, low-dose prednisone is a valuable tool for managing psoriasis flare-ups, but it’s not a standalone solution. A comprehensive approach under the guidance of a dermatologist provides the best results and minimizes long-term risks.
What is Psoriasis and How Does Prednisone Work?
Psoriasis is a chronic autoimmune disease causing rapid skin cell growth, leading to raised, red, scaly patches. These patches commonly appear on the elbows, knees, scalp, and lower back, but can occur anywhere on the body. The severity varies widely.
Prednisone, a corticosteroid, reduces inflammation. It works by suppressing the immune system’s activity, slowing the rapid skin cell turnover characteristic of psoriasis. This lessens the redness, scaling, and itching associated with the condition.
Low-dose prednisone often provides temporary relief, managing symptoms and improving quality of life. However, it’s not a cure and long-term use carries potential side effects, such as increased risk of infection, weight gain, and high blood pressure. Your doctor will carefully monitor your treatment.
Remember to discuss treatment options thoroughly with your dermatologist. They can help determine the best course of action for managing your psoriasis, weighing the benefits of low-dose prednisone against potential risks and alternative therapies.
Low-Dose Prednisone: Dosage and Administration
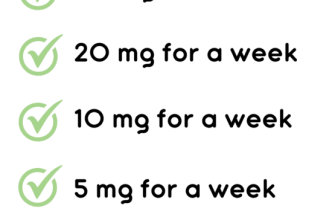
Your doctor will determine the appropriate prednisone dosage based on your individual needs and response to treatment. Typical low-dose prednisone regimens for psoriasis range from 5 to 20 milligrams daily. This is significantly lower than doses used for other conditions.
Administration is usually oral, meaning you’ll take it as a pill with water.
- Timing: Follow your doctor’s instructions regarding the best time to take your medication. Many find it helpful to take it with food to reduce potential stomach upset.
- Duration: Low-dose prednisone for psoriasis is typically prescribed for short periods, often several weeks, to minimize side effects. Your doctor will closely monitor your progress and adjust the dosage or duration as needed.
- Tapering: Never stop taking prednisone suddenly. Your doctor will create a tapering schedule, gradually reducing your dose to avoid withdrawal symptoms. This is a crucial part of treatment.
Some common side effects of prednisone, even at low doses, include weight gain, increased appetite, mood changes, and insomnia. Report any concerning side effects to your physician immediately.
- Consistent Dosing: Taking your prednisone at the same time each day helps maintain consistent blood levels of the medication.
- Missed Doses: If you miss a dose, take it as soon as you remember, unless it’s nearly time for your next dose. Do not double the dose.
- Medication Interactions: Inform your doctor about all other medications, supplements, and herbal remedies you’re taking, as prednisone can interact with some drugs.
Remember, this information is for guidance only. Always follow your doctor’s specific instructions for dosage and administration of your prednisone. They will personalize your treatment plan to optimize results while minimizing risks.
Benefits and Potential Side Effects of Low-Dose Prednisone
Low-dose prednisone can significantly reduce psoriasis symptoms, offering quicker relief than many other treatments. Expect to see improvements in inflammation, redness, and scaling within days to weeks. This rapid response makes it valuable for managing flare-ups. However, remember that low-dose prednisone isn’t a long-term solution; it primarily provides short-term symptom control.
Potential Benefits
Reduced inflammation and itching are common benefits. Many patients report noticeable improvement in skin appearance, leading to improved quality of life. The short-term nature of treatment minimizes cumulative side effects.
Potential Side Effects
While generally well-tolerated at low doses, side effects can occur. Common ones include increased appetite, weight gain, and difficulty sleeping. Less frequent but more serious effects may include increased blood sugar (hyperglycemia) and increased blood pressure. Rarely, low-dose prednisone can cause mood changes or increased risk of infection. Always report any concerning symptoms to your doctor immediately.
Important Note:
Prednisone dosage and duration should be carefully determined by your dermatologist. Never adjust your medication without consulting your doctor. Regular monitoring of blood pressure and blood sugar might be necessary, especially if you have pre-existing conditions.
When is Low-Dose Prednisone Appropriate for Psoriasis?
Low-dose prednisone might be considered for severe psoriasis flare-ups unresponsive to other treatments. Doctors usually prescribe it for short-term management of symptoms, aiming for rapid symptom relief, particularly for those experiencing debilitating flares affecting quality of life.
Specific situations where it’s often considered include:
- Severe erythrodermic psoriasis, covering a large body surface area.
- Psoriatic arthritis causing significant joint pain and inflammation, especially when other medications haven’t provided adequate relief.
- Severe pustular psoriasis, posing a risk of infection.
- Situations requiring rapid symptom control before initiating other systemic treatments like biologics which can take time to work.
Remember: Prednisone is not a long-term solution for psoriasis. Its use is usually limited to short bursts to control severe symptoms, followed by a gradual tapering of the dose to minimize side effects. Your doctor will carefully monitor you for potential adverse events during and after treatment. Alternative or additional treatments are typically explored to manage psoriasis in the long run.
Before considering prednisone, your doctor will assess your overall health, including any other medical conditions you have. They will discuss the risks and benefits, and explore other treatment options first. Prednisone is generally avoided during pregnancy and breastfeeding.
Combining Low-Dose Prednisone with Other Treatments
Low-dose prednisone rarely stands alone in psoriasis treatment. Doctors often prescribe it alongside other therapies to manage symptoms and improve outcomes. This combination approach frequently yields better results than using prednisone by itself.
Topical treatments, like corticosteroids creams or ointments, often complement low-dose prednisone. These target specific affected areas, while prednisone addresses systemic inflammation. This dual approach can significantly reduce redness, scaling, and itching.
Phototherapy, or light therapy, is another effective pairing. UVB or narrowband UVB light treatments reduce inflammation and slow skin cell growth. Combining this with low-dose prednisone allows for lower dosages of each therapy, minimizing potential side effects.
Biologic medications, such as TNF inhibitors or interleukin inhibitors, provide a powerful systemic approach. Prednisone can help manage a flare-up while the biologics work to modify the immune response over the long term. This combination can be particularly beneficial for severe psoriasis cases.
It’s crucial to discuss treatment plans with a dermatologist. They will assess your individual needs and recommend the most suitable combination based on your psoriasis severity, medical history, and other factors. Here’s a table summarizing common combinations:
| Prednisone | Combined Treatment | Benefits |
|---|---|---|
| Low-dose oral | Topical corticosteroids | Targeted symptom relief, reduced inflammation |
| Low-dose oral | Phototherapy (UVB or Narrowband UVB) | Enhanced efficacy, reduced individual dosage requirements |
| Low-dose oral | Biologic medications | Faster flare-up control, long-term immune modulation |
Remember, individual responses to treatment vary. Close monitoring by your dermatologist is key to adjusting the treatment plan as needed and ensuring optimal results. Always follow your doctor’s instructions carefully.
Monitoring Progress and Adjusting Treatment
Schedule regular check-ups with your dermatologist, ideally every 2-4 weeks initially, to track your psoriasis symptoms. We’ll assess your skin’s condition using a Psoriasis Area and Severity Index (PASI) score. This helps quantify improvement.
Expect initial improvements within 1-2 weeks, though full effects might take longer. We’ll adjust your prednisone dosage based on your response. If your psoriasis clears significantly, we’ll consider tapering the dose gradually to minimize side effects.
Careful monitoring is key. Report any new or worsening symptoms, such as increased skin irritation, thinning skin, or changes in mood. We’ll discuss potential side effects and strategies to manage them. These could include medication adjustments or lifestyle modifications.
Blood pressure and blood sugar levels will be monitored regularly, especially if you have a pre-existing condition. Prednisone can affect these, so regular checks are vital. We may request blood tests.
We will collaboratively decide when to discontinue prednisone. A slow tapering schedule usually helps prevent flare-ups and minimizes withdrawal symptoms. We may consider combining prednisone with topical treatments or other systemic therapies for optimal results. We’ll determine the best long-term management plan for your specific needs.
Long-Term Use and Potential Risks
Prolonged prednisone use, even at low doses, carries risks. Doctors carefully weigh the benefits against these potential downsides. Your dermatologist will monitor you closely for any adverse effects. Long-term use can suppress your immune system, making you more susceptible to infections. This increased vulnerability might manifest as frequent colds, flu, or more serious illnesses. Weight gain is another common side effect, often associated with fluid retention and changes in metabolism. Increased blood sugar levels are also possible, potentially impacting individuals with diabetes or predisposing others to the condition. Osteoporosis, a weakening of the bones, is a concern with extended prednisone treatment, increasing fracture risk. Mood changes, such as irritability, anxiety, or depression, can occur. Furthermore, long-term use can lead to hypertension and increased risk of cataracts and glaucoma.
Monitoring Your Health
Regular check-ups are vital during long-term prednisone therapy. Your doctor will likely order blood tests to monitor your blood sugar, blood pressure, and kidney function. Bone density scans may be recommended to assess osteoporosis risk. Open communication with your physician is key; report any new or worsening symptoms immediately. They might adjust your dosage or consider alternative treatments based on your response and any side effects experienced. A gradual tapering off of prednisone is generally recommended to minimize withdrawal symptoms.
Alternative Treatments
Discussions about alternative therapies for psoriasis, like topical treatments, phototherapy, or biologics, should be part of your ongoing care. Your doctor might suggest combining these options with prednisone or transitioning away from it entirely as your psoriasis improves.
Alternative Treatments and Lifestyle Changes
Consider incorporating light therapy, specifically UVB phototherapy, into your treatment plan. Studies show it can significantly reduce psoriasis symptoms for many individuals. Regular sessions, as directed by your dermatologist, are key.
Dietary Adjustments
A diet rich in omega-3 fatty acids, found in fatty fish like salmon, can help reduce inflammation. Limit processed foods, red meat, and dairy – these foods are often associated with increased inflammation. Increase your intake of fruits and vegetables packed with antioxidants.
Stress Management Techniques
Psoriasis flares are often triggered by stress. Practice relaxation techniques such as yoga, meditation, or deep breathing exercises daily. Even 10 minutes a day can make a difference. Consider professional guidance for chronic stress management.
Topical Treatments
Explore natural topical treatments like aloe vera gel or coconut oil. These can soothe irritated skin and reduce itching. Apply them directly to affected areas after showering. Remember to always consult your doctor before trying new topical treatments, especially if you are already using other medications.
Skincare Routine
Maintain a gentle skincare routine. Use mild, fragrance-free cleansers and moisturizers. Avoid harsh soaps and scrubbing. Keep your skin hydrated by showering with lukewarm water and applying moisturizer immediately after drying. Regular exfoliation with a soft brush can help remove dead skin cells.
Exercise and Sleep
Regular exercise boosts your immune system and reduces stress, potentially improving psoriasis. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Prioritize getting 7-8 hours of quality sleep each night – sleep deprivation can exacerbate psoriasis symptoms.
Biologics and Other Medications
While not strictly “alternative,” discuss other psoriasis treatment options with your dermatologist, such as biologics or topical retinoids. These provide targeted relief and may be a beneficial addition to or alternative for low-dose prednisone.