Consult your doctor before combining MMR vaccine with prednisone. Steroids like prednisone can suppress the immune system, potentially reducing the effectiveness of live-attenuated vaccines such as MMR. This means your body might not build adequate immunity after the MMR vaccination.
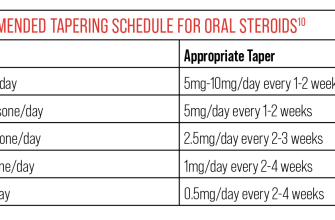
Timing is key. Ideally, avoid administering prednisone within two weeks before or after receiving the MMR vaccine. However, the specific timeframe may depend on your health condition and the prednisone dosage, making discussion with your physician absolutely necessary. They can assess your individual risk profile and advise on the safest approach.
If prednisone use is unavoidable, close monitoring for any unusual symptoms post-vaccination is crucial. Report fever, swelling, or unusual reactions to your doctor promptly. This heightened vigilance compensates for the potential immunosuppressive effects of prednisone and ensures timely intervention if needed.
Remember, this information is for general guidance only. Individual situations vary significantly. Your healthcare provider possesses the necessary expertise to tailor advice based on your specific medical history and current treatment plans. Always prioritize a direct conversation with them before making any decisions regarding your vaccination schedule or medication regimen. Your health is paramount.
MMR Vaccine and Prednisone: Understanding the Interaction
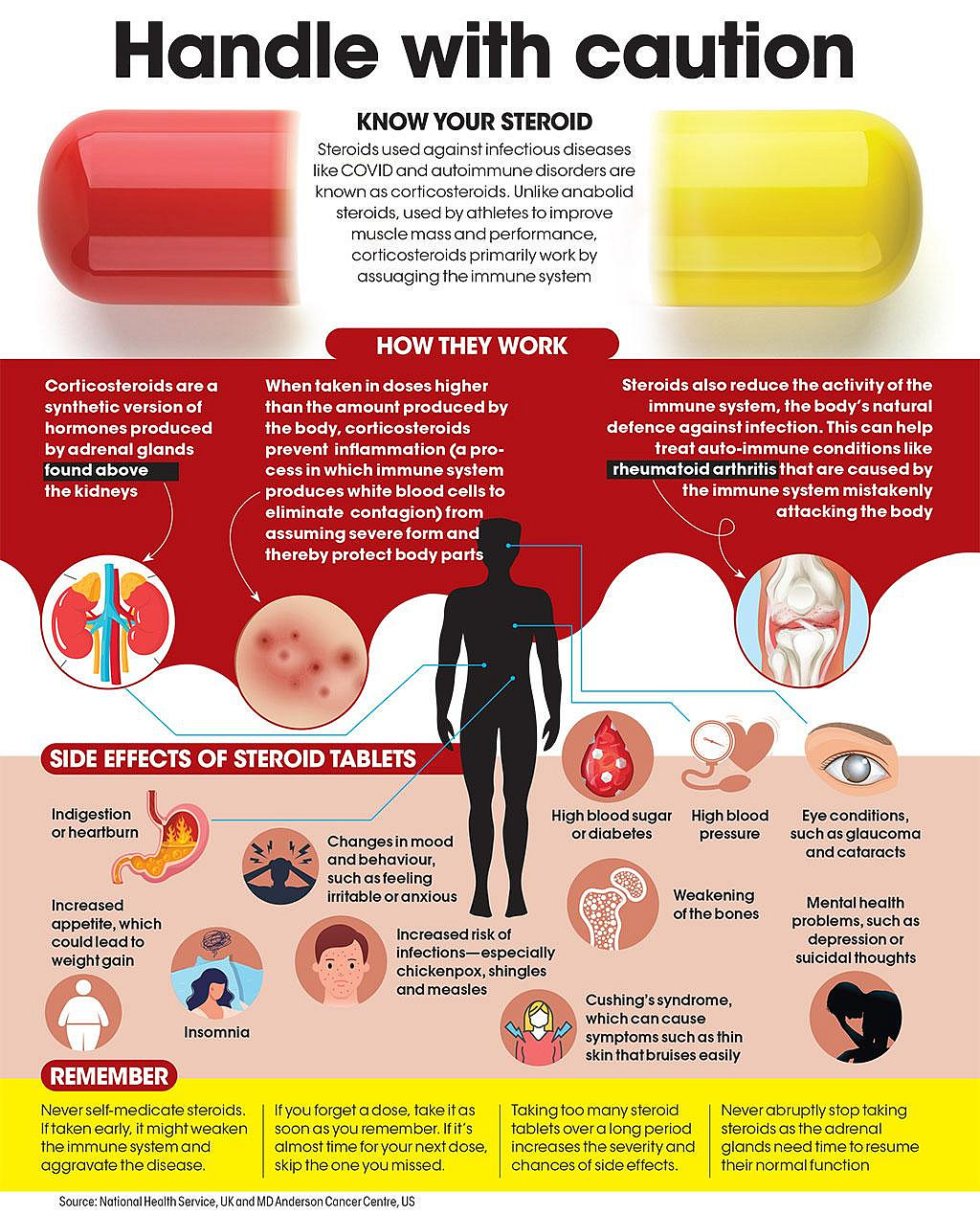
Avoid concurrent administration of the MMR vaccine and prednisone if possible. Prednisone, a corticosteroid, can suppress the immune system’s response to vaccines.
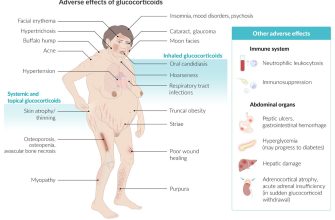
Reduced Immune Response: Prednisone weakens your body’s ability to build immunity. This means the MMR vaccine may be less effective if taken while on prednisone, especially at high doses or for extended durations.
Timing is key: If prednisone treatment is necessary, consult your doctor about delaying the MMR vaccination. The optimal timing depends on the prednisone dosage and duration of treatment. A delay might be recommended until the prednisone course is finished and your immune system has recovered.
Doctor’s Guidance: Always discuss the MMR vaccine with your physician, especially if you are taking prednisone or other immunosuppressants. They can assess your individual circumstances and recommend the best approach. They can also monitor your response to the vaccine.
Alternative Strategies: In some cases, your doctor might adjust your prednisone dosage or consider alternative treatment options to minimize interference with the MMR vaccine. This is particularly true for individuals who have already missed the recommended vaccination schedule and need to catch up.
Monitoring for Adverse Effects: Even with a delayed vaccination, carefully monitor for any adverse reactions after receiving the MMR vaccine. Report any unusual symptoms to your doctor immediately.
Managing MMR Vaccination in Patients on Prednisone: A Practical Guide
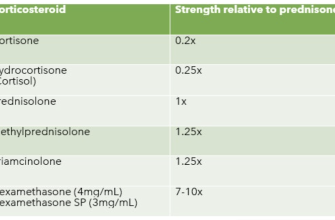
Delay MMR vaccination if possible. Prednisone, especially at high doses or long durations, significantly impairs the immune response. Aim for a prednisone-free period of at least one month before vaccination to maximize effectiveness.
Consult with the patient’s physician. Their medical history and current prednisone regimen inform the safest and most effective vaccination strategy. They can assess individual risk factors and determine the appropriate course of action.
Consider alternative vaccination schedules. If delaying vaccination isn’t feasible, discuss administering the MMR vaccine in two separate doses, spaced further apart than the standard schedule. This might increase the likelihood of a successful immune response.
Monitor for adverse reactions. Closely observe the patient for any signs of infection or unusual reactions post-vaccination. Promptly report any concerns to the treating physician.
Document all vaccination details. Maintain a precise record of the vaccination dates, vaccine lot numbers, and any observed reactions. This information is invaluable for future reference and tracking vaccine efficacy.
Understand that the immune response may be suboptimal. Even with precautions, a weaker immune response is possible due to prednisone. The physician can recommend appropriate follow-up blood tests to assess antibody levels.
Prioritize patient safety. Individualized risk assessment and careful monitoring are critical to ensuring the safest approach for each patient. Always prioritize patient well-being in decision-making.