For most cases of optic neuritis, a high initial dose of prednisone is recommended, typically 1000mg daily. This aggressive approach aims to reduce inflammation quickly and minimize lasting vision impairment.
The duration of this high-dose treatment usually lasts for three days. Following this initial phase, the prednisone dosage is gradually tapered down over several weeks, often by reducing the daily dose by 10-20mg every few days. This careful reduction prevents a sudden relapse and allows your body to adjust. Individual tapering schedules vary based on the severity of your condition and your doctor’s assessment.
Important Note: Oral prednisone carries potential side effects, including increased blood sugar, weight gain, and mood changes. Your physician will monitor your progress closely, adjusting the dosage and duration as needed. Always discuss any concerns or side effects you experience with your doctor promptly.
Remember: This information provides general guidance. The optimal prednisone dosage for optic neuritis is determined on a case-by-case basis by your ophthalmologist or neurologist. They will consider various factors, including your specific symptoms, disease severity, and overall health, to personalize your treatment plan. Always consult with your healthcare provider for personalized advice.
- Optic Neuritis Prednisone Dose: A Detailed Guide
- Standard Prednisone Regimen for Optic Neuritis
- Alternative Regimens
- Adjusting Prednisone Dosage Based on Patient Factors
- Potential Side Effects of Prednisone Treatment
- Gastrointestinal Issues
- Other Potential Side Effects
- Monitoring Progress and Adjusting Treatment
- Visual Acuity and Visual Field Changes
- Modifying Prednisone Dosage
- Alternative Treatments
- Tracking Your Progress
- Important Note:
- Alternative Treatments and Considerations Beyond Prednisone
- Tapering Off Prednisone: A Gradual Approach
Optic Neuritis Prednisone Dose: A Detailed Guide
The standard treatment for optic neuritis involves a high-dose prednisone regimen. Doctors typically prescribe 1000mg of prednisone daily for three days, followed by a tapering schedule. This rapid initial dose aims to reduce inflammation quickly.
Following the initial high dose, the prednisone dose is gradually decreased. A common tapering schedule involves reducing the daily dose by 10-20mg every few days. The exact schedule depends on individual patient responses and the severity of their optic neuritis. Your doctor will personalize your plan.
Some patients may require alternative tapering schedules, perhaps a slower reduction, especially if they experience a relapse or significant side effects. Careful monitoring by your ophthalmologist is key throughout the process.
Important Considerations: Prednisone has potential side effects including weight gain, increased blood sugar, insomnia, and mood changes. Open communication with your doctor about any side effects is critical. They can adjust the dosage or add medication to manage these issues.
Note: This information is for educational purposes only and does not substitute professional medical advice. Always consult your doctor or ophthalmologist for diagnosis and treatment of optic neuritis. They will determine the most appropriate prednisone dose and tapering schedule for your specific case based on your medical history and condition.
Standard Prednisone Regimen for Optic Neuritis
A common treatment involves a high-dose prednisone pulse. This usually starts at 1000 mg daily for three days, followed by a tapering schedule. The tapering schedule gradually reduces the dosage over several weeks. A typical schedule might decrease the dose by 10-20 mg every other day or every three days.
Alternative Regimens
Some doctors may prescribe an oral prednisone regimen of 60-80 mg daily for a week, followed by a gradual taper. Other variations exist, and your doctor will tailor the regimen to your specific needs and response to treatment. Factors like disease severity and personal health will influence the prescribed dosage and duration.
Remember, this information is for educational purposes only and does not constitute medical advice. Always consult your ophthalmologist or neurologist for diagnosis and treatment of optic neuritis. They will consider your individual circumstances when determining the most appropriate prednisone regimen for you.
Adjusting Prednisone Dosage Based on Patient Factors
Prednisone dosage for optic neuritis varies significantly depending on individual patient characteristics. Doctors often begin with a high dose, typically 60-80mg daily, for several days to quickly reduce inflammation. This high initial dose is then tapered gradually over several weeks to minimize side effects.
Age significantly influences dosage adjustments. Older patients, particularly those with pre-existing conditions like diabetes or heart disease, may require lower initial doses and slower tapering schedules to minimize risks of adverse events. Younger patients generally tolerate higher doses better.
Disease severity impacts treatment. Patients with severe vision loss might benefit from a higher initial dose and a longer treatment duration. Conversely, patients with mild optic neuritis may respond well to lower doses and shorter treatment courses.
Concurrent medications must be factored in. Some drugs interact with prednisone, potentially increasing the risk of side effects. Your doctor will carefully consider any other medications you are taking before determining the appropriate prednisone dosage.
Individual responses to prednisone vary widely. Some patients experience significant side effects at lower doses, necessitating dose reductions. Others might need higher doses or longer treatment periods for optimal response. Regular monitoring of both vision and overall health is paramount. Close collaboration with your doctor is key to adjusting the dosage to maximize benefit and minimize harm.
Potential Side Effects of Prednisone Treatment
Prednisone, while effective for optic neuritis, carries potential side effects. These vary in severity and frequency, depending on the dose and duration of treatment. Common side effects include increased appetite leading to weight gain, fluid retention causing swelling (edema), and changes in mood, potentially manifesting as irritability, anxiety, or depression. Some individuals experience insomnia or trouble sleeping.
Gastrointestinal Issues
Prednisone can irritate the stomach lining, causing heartburn, indigestion, or nausea. In more severe cases, ulcers can develop. To mitigate this risk, take prednisone with food. If you experience persistent stomach upset, consult your doctor immediately.
Other Potential Side Effects
Less common, but still possible, side effects include increased blood sugar levels (hyperglycemia), increased blood pressure, thinning of the bones (osteoporosis), and increased susceptibility to infections. High doses or prolonged use increase the likelihood of these occurrences. Regular monitoring of blood pressure and blood sugar is recommended, especially for individuals with pre-existing conditions. Your doctor may also recommend lifestyle modifications to minimize risks, such as dietary adjustments or exercise.
Remember to report any concerning side effects to your doctor promptly. They can adjust your medication or recommend strategies to manage side effects effectively.
Monitoring Progress and Adjusting Treatment
Regularly schedule follow-up appointments with your ophthalmologist. Expect visual acuity tests and visual field examinations at each visit. These assessments track improvements in your vision. Your doctor will also assess your optic nerve’s condition using imaging like OCT (optical coherence tomography).
Visual Acuity and Visual Field Changes
Significant improvements in visual acuity and visual field typically happen within the first few weeks of prednisone treatment. However, recovery can be gradual, extending over several months. A lack of improvement or worsening symptoms warrant adjustments to your treatment plan.
Modifying Prednisone Dosage
Your doctor might consider tapering the prednisone dose slowly if your vision improves steadily. Rapid tapering carries the risk of relapse. Conversely, if your vision doesn’t improve or worsens, they may increase the prednisone dose, potentially adding other medications like immunomodulators.
Alternative Treatments
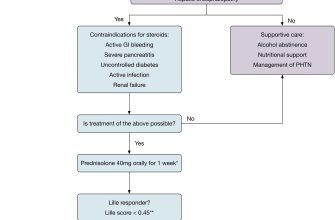
If prednisone proves ineffective or causes significant side effects, alternative treatments such as intravenous corticosteroids or other disease-modifying drugs may be considered. Discuss potential alternative therapies with your doctor to weigh the risks and benefits for your specific situation.
Tracking Your Progress
| Week | Visual Acuity (Right Eye) | Visual Acuity (Left Eye) | Visual Field Changes | Prednisone Dose (mg/day) | Side Effects |
|---|---|---|---|---|---|
| 1 | 20/40 | 20/60 | Mild central scotoma | 60 | None |
| 2 | 20/30 | 20/40 | Improved | 60 | Mild insomnia |
| 4 | 20/25 | 20/30 | Minimal central scotoma | 40 | Insomnia resolving |
| 6 | 20/20 | 20/25 | Normal | 20 | None |
Important Note:
This table is a sample and your individual experience may vary. Close monitoring and communication with your healthcare provider is vital.
Alternative Treatments and Considerations Beyond Prednisone
While prednisone remains a mainstay in optic neuritis treatment, alternative approaches and supplementary therapies exist. These should be discussed with your doctor to determine suitability for your specific case.
- Intravenous Immunoglobulin (IVIG): This treatment involves administering concentrated antibodies intravenously. It’s sometimes used for severe cases or those not responding well to prednisone.
- Plasma Exchange (Plasmapheresis): This procedure removes harmful antibodies from your blood plasma. It’s another option for severe optic neuritis, often considered alongside IVIG.
- Disease-Modifying Therapies (DMTs): If optic neuritis is linked to multiple sclerosis (MS), DMTs like interferon beta, glatiramer acetate, or natalizumab might be prescribed to manage the underlying disease and reduce the risk of future attacks. Your neurologist can evaluate your risk factors and potential benefits of these medications. This approach focuses on the root cause and may prevent relapses, unlike prednisone which addresses the symptoms.
Beyond medication, lifestyle adjustments can help manage symptoms:
- Rest: Adequate rest is critical for visual recovery. Avoid activities that strain your eyes.
- Eye Protection: Sunglasses or protective eyewear can reduce further eye strain and light sensitivity.
- Dietary Considerations: A balanced diet rich in antioxidants and omega-3 fatty acids may support overall health and potentially aid visual recovery. Consult a nutritionist or dietician for personalized guidance.
Remember, early diagnosis and prompt treatment are crucial. Regular follow-up appointments with your ophthalmologist or neurologist are essential for monitoring your condition and adjusting treatment as needed. They will guide you based on your individual health profile and the severity of your optic neuritis.
Tapering Off Prednisone: A Gradual Approach
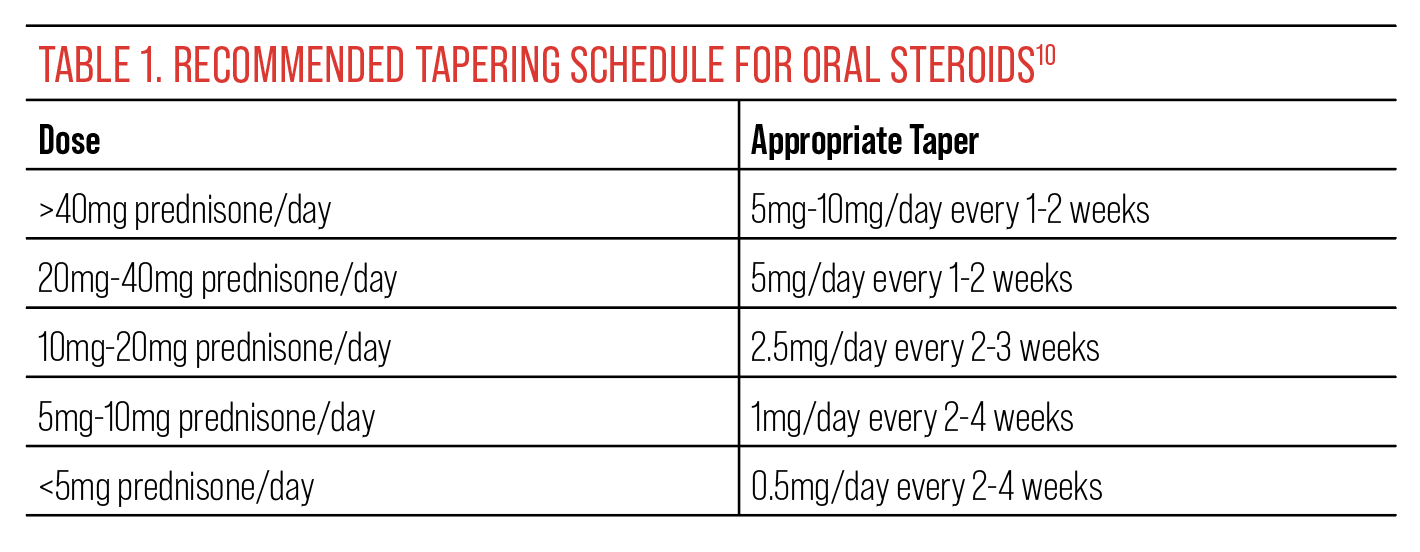
Your doctor will create a personalized prednisone tapering schedule. Generally, this involves gradually reducing your daily dose over several weeks or months. Rapid withdrawal can lead to serious side effects.
Here’s a common approach, but remember, your doctor’s plan is paramount:
- Slow and Steady: Reduce your dosage by a small amount (e.g., 5-10mg) every few days or week, depending on your initial dose and response.
- Alternate-Day Dosing: In some cases, your doctor may recommend taking your full daily dose every other day instead of daily doses. This can help minimize side effects.
- Monitor for Symptoms: Carefully track how you feel. Report any new or worsening symptoms, like fatigue, joint pain, or depression, to your physician immediately.
Specific examples of tapering schedules vary greatly. For instance:
- A patient on 60mg might decrease by 5mg every three days.
- Another might reduce by 10mg every week.
- A third may utilize alternate-day dosing.
The goal is to find the lowest dose that effectively manages your symptoms while minimizing side effects. This process requires close monitoring and collaboration with your doctor. They’ll adjust the schedule based on your individual needs and response to treatment.
Remember: Never stop taking prednisone abruptly without consulting your doctor.