Prednisone offers quick asthma relief, reducing inflammation and opening airways within hours. This makes it invaluable during severe asthma attacks, significantly improving breathing and preventing serious complications. Remember, however, it’s a short-term solution, not a long-term asthma management plan.
Your doctor will likely prescribe prednisone as a course of tablets, often for a short period (e.g., 5-10 days). Precise dosage depends on your individual needs and the severity of your symptoms. Always follow your doctor’s instructions meticulously; never adjust the dosage without consulting them.
Common side effects include increased appetite, weight gain, mood changes, and sleep disturbances. While usually temporary, these effects warrant monitoring. Inform your physician immediately if you experience any concerning side effects or if your symptoms don’t improve after taking the medication.
Long-term prednisone use carries significant risks, including bone thinning, increased susceptibility to infections, and high blood pressure. Therefore, it’s crucial to manage asthma with a long-term plan involving inhalers and other controllers, minimizing reliance on prednisone.
Managing asthma effectively requires a proactive approach. This includes regular check-ups with your doctor, consistent use of prescribed inhalers, and identifying and avoiding your asthma triggers. This combination leads to better control, reducing the frequency of severe attacks and the need for short-term steroid bursts like prednisone.
- Prednisone and Asthma: A Detailed Guide
- Understanding Prednisone’s Role
- Common Side Effects and Management
- Using Prednisone Safely
- Long-Term Asthma Management
- What is Prednisone and How Does it Work for Asthma?
- How Prednisone Works
- Prednisone Dosage and Administration
- Potential Side Effects
- Prednisone and Long-Term Asthma Management
- Short-Term vs. Long-Term Prednisone Use in Asthma Management
- Short-Term Prednisone: Benefits and Considerations
- Long-Term Prednisone: Risks and Alternatives
- Common Side Effects of Prednisone and How to Manage Them
- Gastrointestinal Issues
- Increased Blood Sugar
- Mood Changes
- Fluid Retention and Weight Gain
- Increased Risk of Infection
- Muscle Weakness
- High Blood Pressure
- Thinning Skin
- Cataracts and Glaucoma
- Prednisone and Asthma: Potential Interactions with Other Medications
- When to Seek Immediate Medical Attention While on Prednisone for Asthma
- Signs of Prednisone Side Effects Requiring Attention
- When to Contact Your Doctor
- Tapering Off Prednisone: A Safe and Effective Approach
Prednisone and Asthma: A Detailed Guide
Prednisone, a corticosteroid, effectively reduces asthma inflammation. Doctors prescribe it to control severe asthma attacks or exacerbations. It’s a short-term solution, not a long-term asthma management plan. Always follow your doctor’s instructions precisely regarding dosage and duration.
Understanding Prednisone’s Role
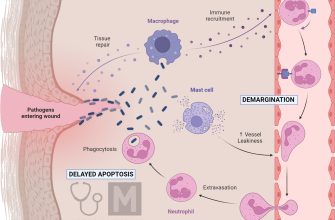
Prednisone works by suppressing the immune system, thus reducing airway swelling and inflammation characteristic of asthma. This leads to improved breathing and reduced symptoms like wheezing and coughing. However, prolonged use carries side effects, so it’s typically used for short bursts to manage flare-ups.
Common Side Effects and Management
Potential side effects include weight gain, increased appetite, mood changes, insomnia, and increased blood sugar. Some people experience fluid retention or increased blood pressure. Your doctor can help you manage these side effects through adjustments in dosage or concurrent medications. Report any concerning symptoms promptly to your physician.
Using Prednisone Safely
Never stop taking prednisone abruptly without consulting your doctor. Sudden cessation can trigger a severe asthma attack. Your doctor will usually taper the dosage gradually to minimize withdrawal symptoms. Regular monitoring of your blood pressure, blood sugar, and weight is advisable while on prednisone. Maintain a healthy lifestyle – including diet and exercise – for optimal results and to mitigate side effects.
Long-Term Asthma Management
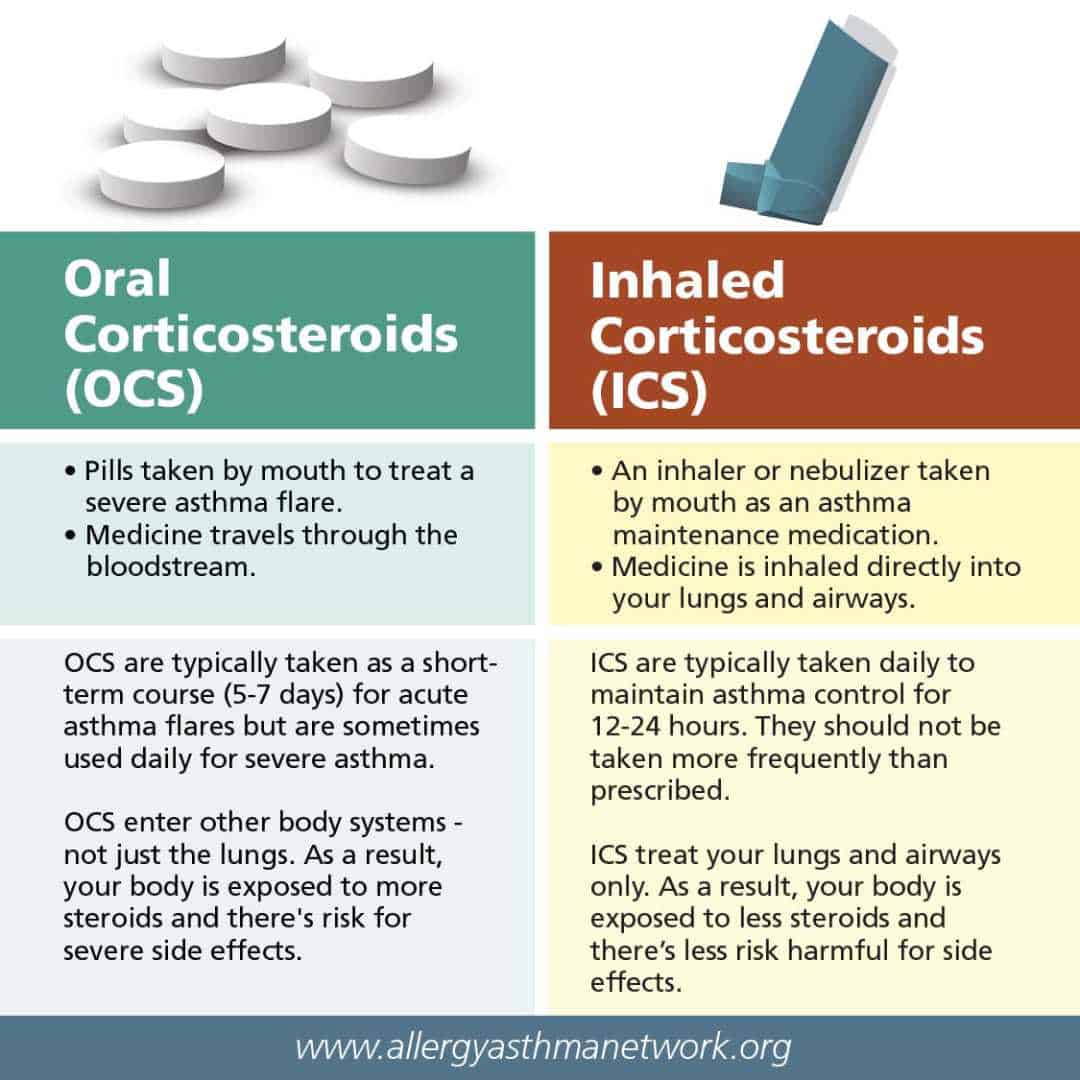
Prednisone isn’t a cure for asthma. Long-term management requires a combination of strategies including inhalers, such as bronchodilators and inhaled corticosteroids, and lifestyle modifications. Your doctor will develop a personalized asthma action plan outlining the best approach for your specific needs. This plan will help you manage your asthma effectively and minimize reliance on oral steroids like prednisone.
What is Prednisone and How Does it Work for Asthma?
Prednisone is a corticosteroid medication, a powerful anti-inflammatory drug. For asthma, it reduces airway swelling and inflammation, providing quick relief from symptoms like wheezing and shortness of breath. It doesn’t prevent asthma attacks, but it effectively manages inflammation already present.
How Prednisone Works
Prednisone works by binding to receptors inside your cells. This interaction triggers a chain reaction, lessening the body’s inflammatory response. Specifically, it reduces the production of inflammatory chemicals, resulting in less swelling and irritation in your airways. This allows you to breathe more easily.
Prednisone Dosage and Administration
Your doctor determines the correct dosage based on your specific needs and the severity of your asthma. Prednisone is usually taken orally, as a tablet or liquid. It’s crucial to follow your doctor’s instructions precisely. Never alter your dosage without consulting your doctor.
| Dosage Form | Administration | Notes |
|---|---|---|
| Tablet | Oral | Swallow whole with water |
| Liquid | Oral | Measure carefully using a provided measuring device |
Potential Side Effects
While Prednisone offers significant benefits, potential side effects include increased appetite, weight gain, mood changes, and increased blood sugar. Long-term use can have more serious side effects. Discuss any concerns with your doctor.
Prednisone and Long-Term Asthma Management
Prednisone is typically used for short-term relief of severe asthma symptoms or exacerbations. It is not usually a long-term solution. Your doctor will likely prescribe other medications, such as inhalers, for ongoing asthma control.
Short-Term vs. Long-Term Prednisone Use in Asthma Management
Prednisone, a corticosteroid, effectively reduces asthma inflammation, but its use depends heavily on the treatment duration. Short-term prednisone courses (typically less than 14 days) are common for managing asthma exacerbations. These bursts provide rapid symptom relief, improving lung function and reducing inflammation. Doctors prescribe this for sudden worsening of asthma symptoms, like increased wheezing or shortness of breath.
Short-Term Prednisone: Benefits and Considerations
Benefits: Quick symptom relief. Considerations: Side effects are generally less pronounced with short courses; however, even brief use can elevate blood sugar, blood pressure, and potentially impact sleep. Regular monitoring is advisable.
Long-Term Prednisone: Risks and Alternatives
Long-term prednisone use (more than 14 days) for asthma is generally avoided due to substantial risks. Prolonged use significantly increases the chance of severe side effects, including osteoporosis, cataracts, weight gain, and increased susceptibility to infections. Inhaled corticosteroids, long-acting beta-agonists, and other asthma control medications provide safer, more sustainable management. Doctors only consider long-term prednisone if other treatments are unsuccessful. Always discuss alternative strategies with your physician.
Remember: This information is for educational purposes only. Always consult your doctor for personalized asthma management. They will assess your individual needs and create a tailored treatment plan.
Common Side Effects of Prednisone and How to Manage Them
Talk to your doctor about any concerns. They can adjust your dosage or suggest ways to mitigate side effects.
Gastrointestinal Issues
Prednisone can upset your stomach. To minimize this, take it with food or milk. If you experience heartburn, consider an antacid. Persistent nausea or vomiting requires immediate medical attention.
Increased Blood Sugar
Monitor your blood sugar regularly, especially if you have diabetes. Your doctor might need to adjust your diabetes medication. Maintain a healthy diet and exercise routine to help control blood sugar levels.
Mood Changes
Some people experience irritability, anxiety, or insomnia. Get enough sleep, engage in relaxing activities like yoga or meditation, and consider talking to a therapist if needed. Your doctor can also discuss medication options to manage mood changes.
Fluid Retention and Weight Gain
Reduce sodium intake to minimize fluid retention. Drink plenty of water to support kidney function. A balanced diet and regular exercise can help manage weight gain. Remember, weight fluctuations are a common side effect.
Increased Risk of Infection
Practice good hygiene, avoid crowds during illness outbreaks, and tell your doctor immediately if you feel unwell. Prednisone weakens your immune system, making you more susceptible to infections. Early intervention is key.
Muscle Weakness
Engage in gentle exercise to maintain muscle strength and bone density, but avoid strenuous activity. A balanced diet rich in calcium and vitamin D is important. Your doctor can advise on appropriate exercise levels.
High Blood Pressure
Monitor your blood pressure regularly. A low-sodium diet, regular exercise, and stress reduction techniques can all help. Your doctor might prescribe medication to manage blood pressure if necessary. This is particularly important if you have pre-existing hypertension.
Thinning Skin
Use a gentle moisturizer regularly to keep your skin hydrated and protect it from sun damage. Always use sunscreen with a high SPF. This minimizes the risk of bruising and skin tears.
Cataracts and Glaucoma
Regular eye exams are recommended, especially if you have a history of eye problems. Your doctor can monitor your eye health and discuss the long-term impact of Prednisone on your vision. Early detection is crucial for optimal treatment.
Prednisone and Asthma: Potential Interactions with Other Medications
Always inform your doctor about all medications you take, including over-the-counter drugs, supplements, and herbal remedies, before starting prednisone. This includes prescription asthma medications like inhaled corticosteroids (e.g., fluticasone, budesonide) and bronchodilators (e.g., albuterol, salmeterol).
Prednisone can increase blood sugar levels, so it’s crucial to monitor this if you’re taking diabetes medication (e.g., insulin, metformin). Adjustments to your diabetes regimen might be necessary.
Simultaneous use of prednisone and certain medications can increase the risk of bleeding. Examples include blood thinners (e.g., warfarin, aspirin) and nonsteroidal anti-inflammatory drugs (NSAIDs, e.g., ibuprofen, naproxen). Close monitoring for bleeding is advised.
Prednisone may affect the effectiveness of some vaccines, potentially diminishing their immune response. Discuss vaccination schedules with your doctor.
Interactions with medications affecting potassium levels (e.g., diuretics, some heart medications) also need consideration, as prednisone can impact potassium balance. Your doctor will monitor your potassium levels.
Prednisone can weaken bones, so combining it with medications that also increase bone loss risk (e.g., some anticonvulsants) requires careful assessment. Your doctor might recommend supplemental calcium and vitamin D.
Be aware that this list isn’t exhaustive. Discuss all your medications with your physician or pharmacist to identify and manage potential drug interactions safely.
When to Seek Immediate Medical Attention While on Prednisone for Asthma
Seek immediate medical attention if you experience any of the following:
- Severe breathing difficulty: This includes wheezing that doesn’t improve with your inhaler, struggling to catch your breath, or feeling like you can’t get enough air.
- Rapid heart rate: A significantly increased heart rate accompanied by shortness of breath warrants immediate medical evaluation.
- Chest pain: Chest pain, especially if it’s severe or accompanied by shortness of breath, requires immediate attention.
- Significant worsening of asthma symptoms: If your usual asthma management plan is ineffective, and symptoms dramatically worsen despite medication, contact your doctor immediately. This includes needing to use your rescue inhaler much more frequently than usual.
- Signs of infection: High fever, chills, increased cough, or worsening of lung sounds may indicate a respiratory infection requiring urgent care. Prednisone can suppress your immune system, making infections more dangerous.
- Severe allergic reaction: Symptoms like hives, swelling of the face or throat (angioedema), or difficulty swallowing indicate a potentially life-threatening allergic reaction.
- Mental status changes: Confusion, disorientation, or unusual behavior can be related to high doses of prednisone and necessitate prompt medical assessment.
Signs of Prednisone Side Effects Requiring Attention
While not always emergencies, certain side effects should prompt contact with your doctor:
- Significant weight gain: Sudden, substantial weight gain can be a side effect of prednisone.
- Increased blood sugar: Monitor blood sugar levels, especially if you have diabetes. Report significant changes to your doctor.
- Mood swings: Prednisone can affect mood. If you experience significant irritability, anxiety, or depression, contact your doctor.
- Increased blood pressure: Regularly monitor your blood pressure and report significant increases to your doctor.
- Muscle weakness: Unusual muscle weakness or pain should be reported.
- Difficulty sleeping: Insomnia or sleep disturbances, especially persistent ones, warrant attention.
When to Contact Your Doctor
Beyond immediate emergencies, contact your doctor for any concerns regarding your asthma or prednisone treatment. Regular communication is vital for managing your condition effectively.
Tapering Off Prednisone: A Safe and Effective Approach
Never stop Prednisone abruptly. Always follow your doctor’s instructions for a gradual reduction.
Your doctor will create a personalized tapering schedule, typically involving small, regular decreases in your dosage. This might mean lowering your dose by a specific amount every few days or weeks. Closely monitor your symptoms throughout the process.
- Common tapering schedules include decreasing the dose by 5-10mg every few days to a week, depending on the initial dose and your response.
- Longer tapering periods, potentially extending over several weeks or even months, are sometimes necessary for higher initial doses or individuals with more severe asthma.
During tapering, you might experience withdrawal symptoms like fatigue, joint pain, or worsening asthma symptoms. These are common and usually resolve with continued careful reduction. Report any concerning symptoms immediately to your doctor.
- Increased fatigue: Rest more, pace yourself, and consider adjusting your activity level.
- Joint pain: Talk to your doctor about pain management strategies.
- Worsening asthma: Ensure you continue using your inhalers as prescribed and contact your doctor promptly for adjustments.
Your doctor might also suggest increasing the dose of your maintenance asthma medication during the tapering period to minimize the risk of exacerbation. Regular monitoring of your lung function (through peak flow measurements or spirometry) will help track your progress and identify potential problems.
Successful tapering requires close collaboration with your doctor. Open communication is key; don’t hesitate to express any concerns or difficulties you encounter. They will provide guidance and adjust the tapering plan as needed, ensuring a safe and successful transition to your maintenance medication. Regular check-ups are crucial to monitor your progress and adapt the treatment accordingly.