Prednisone, while effective for reducing inflammation, can interact significantly with epilepsy medications and potentially trigger seizures. Close monitoring of seizure activity is crucial during and after Prednisone treatment. Consult your neurologist before starting any Prednisone regimen if you have epilepsy.
The mechanism behind this interaction isn’t fully understood, but evidence suggests Prednisone’s impact on hormone levels and liver enzyme activity can alter the metabolism of anti-epileptic drugs (AEDs). This can lead to either reduced AED effectiveness or increased risk of side effects due to elevated drug concentrations. Regular blood tests to monitor AED levels are highly recommended throughout the Prednisone course.
Specific AEDs are affected differently. For example, Prednisone may increase the metabolism of certain AEDs, requiring a dosage adjustment. Conversely, it may inhibit the metabolism of others, potentially increasing their levels and the risk of adverse reactions. Your doctor will work with you to establish a safe and effective treatment plan, tailored to your individual needs and medication profile. Open communication with your healthcare team is paramount.
Remember: Never adjust your AED dosage without consulting your doctor. Report any changes in seizure frequency or severity, or any new symptoms immediately. Proactive monitoring and open communication are key to managing the potential complications associated with concurrent Prednisone and AED use.
- Prednisone and Epilepsy: A Detailed Look
- Prednisone’s Effects on AEDs
- Managing the Interaction
- Potential Seizure Exacerbation
- Prednisone’s Mechanism of Action and Potential Effects on Seizures
- Impact on GABA and Glutamate
- Clinical Considerations
- Prednisone and Epilepsy: Interactions and Considerations for Patients on Anti-Epileptic Drugs
- Using Prednisone in Epilepsy Treatment: Specific Situations and Guidelines
- Status Epilepticus
- Sudden Seizure Worsening
- Specific Guidelines & Cautions
- Monitoring Key Parameters
- Other Considerations
- Potential Side Effects of Prednisone in Patients with Epilepsy
- Managing Prednisone Use in Epilepsy: Monitoring and Tapering Strategies
- Long-Term Effects and Considerations for Epilepsy Patients
- Bone Health and Prednisone
- Mental Health Impacts
- Managing Other Epilepsy Medications
- Tapering Off Prednisone
Prednisone and Epilepsy: A Detailed Look
Prednisone, a corticosteroid, can interact with epilepsy medications and potentially affect seizure control. This interaction is complex and depends heavily on several factors, including the specific anti-epileptic drug (AED) used, the prednisone dosage, and the individual’s unique metabolism.
Prednisone’s Effects on AEDs
Prednisone can induce hepatic enzymes. This means it can speed up the breakdown of some AEDs in the liver, leading to lower blood levels of the AED and potentially increased seizure frequency. Conversely, prednisone might also interact with other AEDs by altering their absorption or distribution. Close monitoring of seizure activity and AED blood levels is vital during prednisone treatment, especially in the initial stages and any dosage changes.
Managing the Interaction
Consult your doctor or neurologist *before* starting prednisone if you have epilepsy. They can adjust your AED dosage as needed to maintain therapeutic levels while on prednisone. Regular blood tests to monitor AED levels are usually recommended. Be sure to report any changes in seizure frequency or intensity to your healthcare provider immediately. They might need to adjust your medication or treatment plan. Open communication with your medical team is key for effective management.
Potential Seizure Exacerbation
While prednisone’s enzyme-inducing effect is a primary concern, prednisone itself can also have a direct effect on brain activity, potentially increasing seizure risk in susceptible individuals. The risk is particularly heightened in those with poorly controlled epilepsy or pre-existing neurological conditions. This potential effect highlights the importance of careful monitoring and proactive communication with your doctor.
Prednisone’s Mechanism of Action and Potential Effects on Seizures
Prednisone, a glucocorticoid, reduces inflammation by binding to intracellular receptors, influencing gene transcription. This affects various processes, including immune response modulation. Higher doses might increase the seizure threshold in some individuals by influencing GABAergic and glutamatergic neurotransmission.
Impact on GABA and Glutamate
Prednisone’s effects on GABA and glutamate systems are complex and not fully understood. Some studies suggest it can enhance GABAergic inhibition, potentially reducing neuronal excitability and thus seizure activity. Conversely, other research indicates possible glutamate-mediated effects that could potentially increase seizure risk. These varying effects likely depend on dosage, duration of use, and individual patient factors.
Clinical Considerations
Clinicians should carefully monitor patients with epilepsy prescribed prednisone for other conditions. Regular seizure monitoring is crucial. Dose adjustments and careful consideration of alternative therapies are necessary, particularly for those with pre-existing seizure disorders or a history of increased seizure frequency. A thorough understanding of the patient’s specific condition and potential risks is vital. Consult medical literature for updated information on the precise effects of Prednisone on different seizure types.
Prednisone and Epilepsy: Interactions and Considerations for Patients on Anti-Epileptic Drugs
Consult your doctor immediately if you are prescribed prednisone while taking anti-epileptic drugs (AEDs).
Prednisone, a corticosteroid, can interact with many AEDs, potentially altering their effectiveness. This interaction can lead to either a decreased or increased concentration of the AED in your bloodstream, impacting seizure control.
- Reduced AED Effectiveness: Prednisone can induce liver enzymes, speeding up the metabolism of some AEDs. This means your body breaks down the medication faster, reducing its levels and potentially increasing the risk of seizures. Examples of AEDs affected include phenytoin and carbamazepine.
- Increased AED Effectiveness: In some cases, prednisone might slow down the metabolism of certain AEDs, resulting in higher blood levels. This can lead to an increased risk of side effects associated with those AEDs. This is less common but still important to monitor.
Therefore, regular blood tests to monitor AED levels are crucial while taking prednisone concurrently. Your doctor will adjust your AED dosage accordingly to maintain therapeutic levels and minimize risks.
- Close Monitoring: Expect frequent blood draws to check your AED levels. This allows for timely dosage adjustments.
- Dosage Adjustments: Be prepared for your doctor to change your AED dose. This is a proactive step to maintain seizure control.
- Symptom Tracking: Carefully track any changes in seizure frequency, intensity, or the emergence of new symptoms. Report any concerns immediately.
Prednisone itself can also have side effects, some of which can mimic epilepsy symptoms. These include mood changes, insomnia, and even hallucinations. It’s imperative to differentiate between prednisone side effects and changes related to your epilepsy.
Remember, open communication with your healthcare provider is key. Discuss all medications you’re taking, including over-the-counter drugs and supplements, to ensure safe and effective management of your epilepsy while on prednisone.
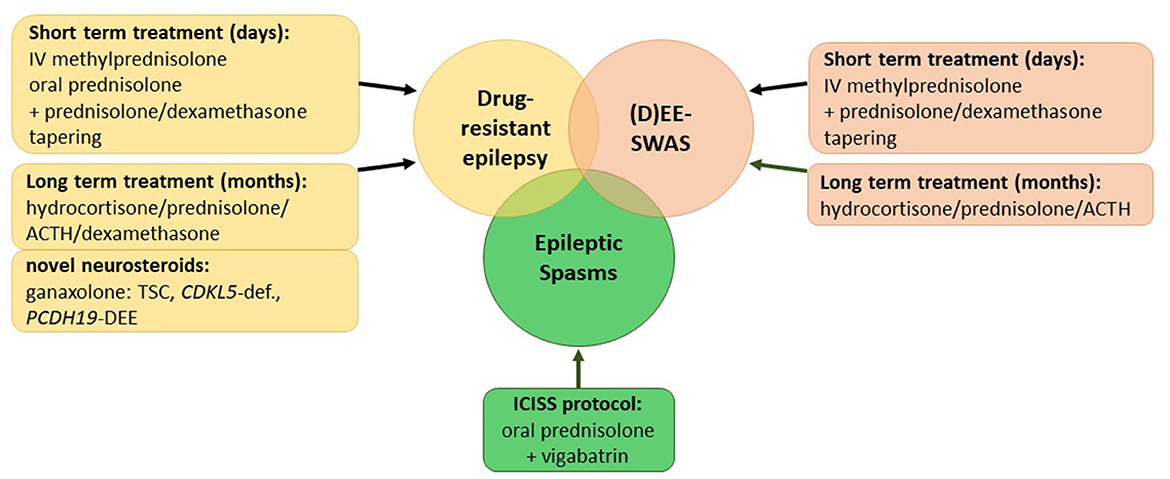
Using Prednisone in Epilepsy Treatment: Specific Situations and Guidelines
Prednisone’s role in epilepsy management is primarily adjunctive, meaning it supports other treatments, not replacing them. It’s most often used to manage acute situations like status epilepticus or to control seizures worsening suddenly. Avoid using it for long-term seizure control due to significant side effects.
Status Epilepticus
In status epilepticus, a life-threatening condition of prolonged seizures, high-dose intravenous prednisone may be administered, often in conjunction with other anticonvulsants. Dosage and duration depend heavily on the patient’s condition and response, guided by a neurologist. Close monitoring for side effects, including increased blood sugar and blood pressure, is absolutely necessary.
Sudden Seizure Worsening
If a patient experiences a sudden, significant increase in seizure frequency or severity despite established anti-epileptic drug (AED) therapy, a short course of prednisone might be considered. This isn’t a first-line option; potential causes like infection or medication interactions need to be ruled out first. The neurologist will tailor the prednisone regimen to the individual circumstances. Careful monitoring for side effects remains paramount.
Specific Guidelines & Cautions
Remember, prednisone use demands careful consideration. Weeding out other potential causes for seizure exacerbation is essential before initiating treatment. Gradual tapering of prednisone is always recommended to minimize withdrawal effects.
Monitoring Key Parameters
| Parameter | Frequency of Monitoring | Why it Matters |
|---|---|---|
| Blood Glucose | Daily, especially initially | Prednisone can elevate blood sugar |
| Blood Pressure | Regularly | Prednisone can increase blood pressure |
| Weight | Weekly | Monitor for fluid retention |
| Seizure Frequency | Daily log | Track treatment effectiveness |
Other Considerations
Patients with a history of certain conditions, such as glaucoma, peptic ulcers, or diabetes, require additional monitoring while on prednisone. Open communication with your doctor about all medications, including over-the-counter drugs and herbal supplements, is vital. Always report any new or worsening symptoms. Prednisone should only be used under the direct supervision of a neurologist.
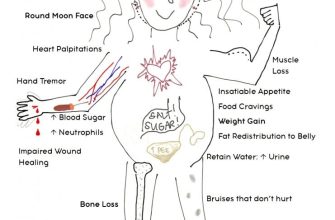
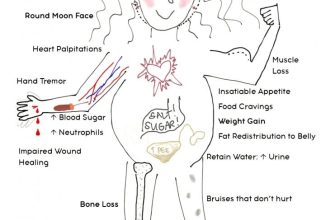
Potential Side Effects of Prednisone in Patients with Epilepsy
Prednisone, while effective for many conditions, can interact with epilepsy medications and cause additional side effects. Careful monitoring is key.
Here’s what you should be aware of:
- Increased Seizure Frequency: Prednisone can sometimes lower the effectiveness of anti-seizure medications, potentially leading to more frequent or severe seizures. Regular monitoring by your doctor is vital.
- Mood Changes: Mood swings, irritability, anxiety, and even depression are possible. Open communication with your doctor and support system is crucial if these occur.
- Insomnia: Difficulty sleeping is a common side effect. Discuss sleep hygiene strategies with your doctor and consider any adjustments to your medication schedule.
- Gastrointestinal Issues: Stomach upset, heartburn, and ulcers are potential concerns. Your doctor may recommend strategies to mitigate these, such as antacids or dietary modifications.
- Weight Gain: Fluid retention and increased appetite can contribute to weight gain. Maintaining a healthy diet and exercise routine can help manage this.
- Increased Blood Sugar: Prednisone can elevate blood sugar levels, posing a particular risk for individuals with diabetes. Regular blood sugar monitoring is necessary.
- Osteoporosis: Long-term prednisone use can weaken bones, increasing the risk of fractures. Discuss bone density testing and preventative measures with your doctor.
- Increased Blood Pressure: Prednisone may raise blood pressure. Regular blood pressure checks are crucial.
It’s imperative to report any new or worsening symptoms to your doctor immediately. They can adjust your medication or treatment plan as needed.
Remember, this information is for general knowledge and should not replace advice from your healthcare provider. Always consult your doctor before starting, stopping, or changing any medication.
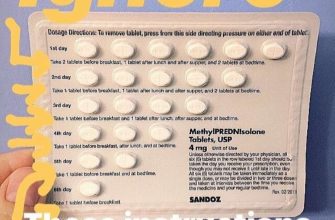
Managing Prednisone Use in Epilepsy: Monitoring and Tapering Strategies
Closely monitor your blood pressure, blood sugar, and weight regularly during prednisone treatment. Report any significant changes to your doctor immediately.
Regular blood tests help track potential side effects like increased risk of infection. Your doctor will schedule these based on your individual needs and response to the medication.
Prednisone can affect bone density. Discuss bone density testing with your doctor, especially if you’re on prednisone for an extended period.
Tapering prednisone is crucial to minimize withdrawal symptoms. Never stop prednisone abruptly. Your doctor will create a gradual tapering schedule, often reducing the dose slowly over weeks or months, depending on the duration of your treatment and your body’s response.
Typical tapering schedules involve small, incremental decreases in dosage. For example, a 5mg reduction every few days or a 10mg reduction per week, but the specifics depend entirely on your doctor’s assessment.
During tapering, carefully monitor for symptoms like fatigue, muscle weakness, and joint pain. Report these to your doctor immediately, as adjustments to the tapering schedule may be necessary.
Maintaining a healthy diet and regular exercise can help mitigate some prednisone side effects and support your overall health during and after treatment.
Open communication with your doctor is vital. Don’t hesitate to ask questions or express concerns about side effects or the tapering process. Your doctor’s guidance is paramount for safe and effective prednisone management.
Long-Term Effects and Considerations for Epilepsy Patients
Regularly monitor your blood sugar levels, as Prednisone can elevate them, potentially leading to hyperglycemia. Discuss dietary adjustments and possible medication changes with your doctor. Regular blood pressure checks are also vital, because Prednisone can increase blood pressure. Your doctor can adjust your medication or recommend lifestyle modifications.
Bone Health and Prednisone
Prednisone can weaken bones, increasing the risk of fractures. Consume a calcium-rich diet, consider calcium and vitamin D supplements, and engage in weight-bearing exercise. Your physician may recommend a bone density scan to monitor bone health.
Mental Health Impacts
Some patients experience mood changes, such as anxiety or depression, while taking Prednisone. Openly communicate any emotional shifts with your doctor; they can offer strategies for managing these side effects, including medication adjustments or referral to a mental health professional. Report any unusual behavior or thoughts immediately.
Managing Other Epilepsy Medications
Prednisone can interact with other epilepsy medications. Always inform your neurologist and pharmacist about all medications you are taking, including over-the-counter drugs and supplements. They can assess potential interactions and adjust dosages accordingly. Never abruptly stop taking your epilepsy medications without your doctor’s guidance.
Tapering Off Prednisone
Abruptly stopping Prednisone can cause withdrawal symptoms. Your doctor will create a tapering schedule to minimize the risk of these issues. Carefully follow their instructions and report any unusual symptoms. This process takes time and requires patience.