Prednisone, while highly effective for managing inflammation, can interfere with iron absorption, leading to deficiency. This often manifests as fatigue and weakness, impacting daily life. Monitor your iron levels regularly if you’re on prednisone; blood tests provide the most accurate assessment.
Dietary changes can significantly mitigate this risk. Prioritize iron-rich foods like red meat, spinach, and lentils. Pairing these with vitamin C enhances absorption. Consider a diet journal to track your intake and identify areas for improvement. Your doctor can also advise on supplements if necessary, but always discuss this beforehand.
Long-term prednisone use increases the likelihood of iron deficiency. Regular check-ups with your physician are vital for early detection and intervention. They can adjust your prednisone dosage or recommend supportive therapies if problems arise, ensuring you maintain optimal health. Proactive management is key.
Remember: This information is for educational purposes and does not replace professional medical advice. Always consult your doctor before making changes to your medication or diet. Open communication with your healthcare provider is paramount for managing both your prednisone treatment and any related iron deficiency.
- Prednisone and Iron Deficiency: A Complex Relationship
- How Prednisone Affects Iron Absorption
- Impact on Iron-Binding Proteins
- Practical Implications and Recommendations
- Potential Interactions with Other Medications
- Prednisone’s Impact on Red Blood Cell Production
- Understanding the Mechanism
- Potential Consequences and Management
- Symptoms of Iron Deficiency While on Prednisone
- Differentiating Prednisone Side Effects from Iron Deficiency
- Diagnosing Iron Deficiency in Prednisone Users
- Further Investigations
- Interpreting Results
- Important Considerations
- Managing Iron Deficiency During Prednisone Treatment
- Lifestyle Changes to Support Iron Levels
Prednisone and Iron Deficiency: A Complex Relationship
Prednisone, a common corticosteroid, can interfere with iron absorption and increase iron loss, leading to iron deficiency anemia. This isn’t a simple cause-and-effect; several factors contribute to the complexity.
- Reduced Iron Absorption: Prednisone alters gut function, impacting the absorption of iron from food. This effect is most pronounced with non-heme iron (found in plant-based foods), which is already less readily absorbed than heme iron (from animal sources).
- Increased Iron Loss: Prednisone can increase blood loss through gastrointestinal irritation, potentially exacerbating pre-existing iron deficiencies.
- Hepcidin Influence: Prednisone affects hepcidin, a hormone regulating iron release from stores. High hepcidin levels, often induced by prednisone, can lock iron away, making it unavailable for red blood cell production.
Consequently, individuals taking prednisone, particularly those already at risk for iron deficiency (e.g., vegetarians, those with heavy menstrual bleeding), should monitor their iron levels regularly. Regular blood tests are key.
- Consult your doctor: Discuss your prednisone use and iron levels with your physician. They can assess your risk and recommend appropriate testing.
- Dietary Adjustments: Consume iron-rich foods. Pair plant-based iron sources with vitamin C to enhance absorption. Examples include spinach with lemon juice or lentils with orange slices.
- Iron Supplements: Your doctor may prescribe an iron supplement, possibly a type that bypasses the gut absorption issues. Never start iron supplements without medical guidance.
Proper monitoring and proactive management minimize the risks of iron deficiency during prednisone treatment. Remember, individual responses vary, so personalized medical advice is critical. Don’t hesitate to contact your healthcare provider with any concerns.
How Prednisone Affects Iron Absorption
Prednisone, a corticosteroid, interferes with iron absorption in the gut. This happens because it reduces the production of hepcidin, a hormone that regulates iron release from stores. While less hepcidin might seem beneficial for iron levels, it’s complicated. Increased iron release from stores can actually worsen inflammation, a condition prednisone is often prescribed for.
Impact on Iron-Binding Proteins
Prednisone also impacts transferrin, the protein that carries iron in the bloodstream. High prednisone doses can increase transferrin levels, but this doesn’t always translate to better iron uptake by your body’s cells. Conversely, low transferrin saturation suggests that even though iron might be available, your body isn’t efficiently using it.
Practical Implications and Recommendations
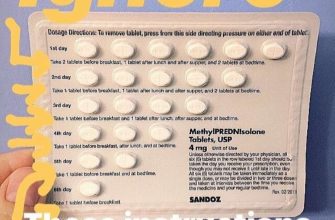
Regular blood tests monitoring your iron levels (ferritin, serum iron, transferrin saturation) are crucial while taking prednisone. Your doctor may recommend iron supplements, but timing is important. Iron absorption is best when taken separately from prednisone, often several hours apart. Consider dietary changes to improve iron intake; foods rich in heme iron (from animal sources) are more easily absorbed than non-heme iron (from plant sources). Consuming iron-rich foods with Vitamin C enhances absorption.
Potential Interactions with Other Medications
Important: Prednisone can interact with other medications, affecting iron absorption. Discuss all your medications with your doctor or pharmacist to minimize potential negative impacts. For example, some antacids can reduce iron absorption.
Prednisone’s Impact on Red Blood Cell Production
Prednisone, a corticosteroid, can suppress red blood cell production (erythropoiesis). This happens because it interferes with the hormone erythropoietin, a key regulator of red blood cell formation in the bone marrow. Reduced erythropoietin levels lead to decreased red blood cell production.
Understanding the Mechanism
Prednisone’s effect isn’t direct. It indirectly impacts erythropoietin production by influencing the kidneys, the primary site of erythropoietin synthesis. High doses of prednisone, or prolonged use, are more likely to cause this suppression. The severity varies depending on factors such as the dosage, duration of treatment, and individual patient response. Monitoring blood counts regularly is critical.
Potential Consequences and Management
Decreased red blood cell production can manifest as anemia, characterized by fatigue, weakness, and shortness of breath. Regular blood tests, including complete blood counts (CBCs), are necessary to monitor hemoglobin levels and identify potential anemia. If anemia develops, your doctor may adjust your prednisone dosage or prescribe erythropoiesis-stimulating agents (ESAs) to help stimulate red blood cell production. Dietary modifications, focusing on iron-rich foods, might also be recommended. Open communication with your doctor is vital for managing potential side effects.
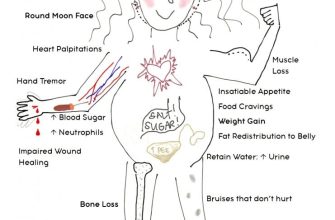
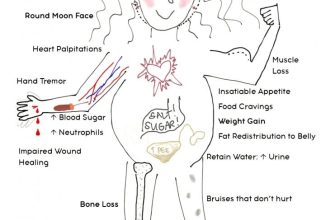
Symptoms of Iron Deficiency While on Prednisone
Prednisone can interfere with iron absorption, increasing your risk of deficiency. Watch for these common signs: unexplained fatigue, weakness, shortness of breath, dizziness, headaches, pale skin, brittle nails, and hair loss. These symptoms might mimic prednisone side effects, making diagnosis tricky.
Differentiating Prednisone Side Effects from Iron Deficiency
Fatigue is a common side effect of both prednisone and iron deficiency. However, iron deficiency often presents with additional symptoms like pale conjunctiva (the white part of your eye) and pica (craving non-nutritive substances). If you experience these, consult your doctor immediately. They can order blood tests to determine your iron levels and differentiate between the two.
Remember, prompt medical attention is key. Don’t self-diagnose or self-treat. Your doctor will help you manage both your prednisone treatment and any iron deficiency.
Diagnosing Iron Deficiency in Prednisone Users
Consult your doctor for iron deficiency testing. They will likely order a complete blood count (CBC) to measure your hemoglobin and hematocrit levels. Low levels suggest anemia, a common sign of iron deficiency.
Further Investigations
If your CBC shows anemia, your doctor might order a serum ferritin test. Ferritin is a protein that stores iron in your body. Low ferritin levels directly indicate low iron stores. They may also test your transferrin saturation, which measures how much iron your transferrin protein is carrying. Low transferrin saturation, alongside low ferritin, strengthens the diagnosis. A soluble transferrin receptor (sTfR) test can help distinguish iron deficiency from other causes of anemia.
Interpreting Results
Remember: Interpreting these tests requires medical expertise. Your doctor will consider your symptoms, medical history, and prednisone dosage when making a diagnosis. Don’t self-diagnose or self-treat. Low iron levels in the context of prednisone use need careful evaluation to determine the underlying cause and appropriate treatment.
Important Considerations
Prednisone itself can interfere with iron absorption, so it’s crucial to discuss potential drug interactions with your doctor when considering iron supplementation. They can help you find the right type of iron supplement and the correct dosage to avoid complications. Regular monitoring of your iron levels while taking prednisone is important, even after iron levels have improved.
Managing Iron Deficiency During Prednisone Treatment
Monitor your iron levels regularly with blood tests, as prescribed by your doctor. Prednisone can interfere with iron absorption and increase your risk of deficiency.
Discuss iron supplementation with your doctor. They can determine the appropriate type and dosage of iron supplement, considering your specific needs and potential interactions with prednisone. Oral iron supplements are common, but intravenous iron may be necessary in cases of severe deficiency.
- Consider your diet. Increase your intake of iron-rich foods like red meat, spinach, lentils, and beans.
- Optimize iron absorption. Consume iron-rich foods with Vitamin C, which enhances absorption. Avoid taking iron supplements with calcium or antacids, as these can hinder absorption.
- Address underlying causes. If your doctor identifies other contributing factors to your iron deficiency, treat those conditions to improve your iron levels.
Report any symptoms of iron deficiency anemia, such as fatigue, weakness, shortness of breath, or pale skin, to your doctor immediately. Early intervention is key to managing iron deficiency effectively during prednisone treatment.
- Regular blood tests are your best ally in monitoring your progress.
- Close communication with your doctor ensures tailored treatment based on your response.
- Active participation in your care, including dietary changes, significantly impacts outcomes.
Remember, successful management requires a team approach: your doctor, you, and your commitment to a personalized treatment plan.
Lifestyle Changes to Support Iron Levels
Prioritize iron-rich foods. Include lean red meat, poultry, fish, beans, lentils, spinach, and fortified cereals in your diet daily. Aim for a variety of sources to maximize absorption.
Enhance iron absorption. Consume vitamin C-rich foods alongside iron-containing meals. Examples include oranges, strawberries, and bell peppers. Avoid drinking tea or coffee with meals, as they hinder iron absorption.
Consider your cooking methods. Iron cookware can subtly increase the iron content of your food. Avoid using antacids containing calcium or aluminum, which can interfere with iron absorption.
Manage your gut health. A healthy gut microbiome is crucial for nutrient absorption. Focus on a diet rich in fiber and prebiotics, and consider a probiotic supplement after consulting your doctor.
| Food | Iron (mg) per serving |
|---|---|
| 3 oz cooked beef | 3 mg |
| 1 cup cooked lentils | 6 mg |
| 1 cup cooked spinach | 6 mg |
| 1/2 cup fortified cereal | 8 mg (varies by brand) |
Schedule regular check-ups. Monitor your iron levels through regular blood tests, especially if you’re taking Prednisone. Your doctor can provide personalized guidance based on your results.
Address underlying conditions. Certain medical conditions, such as celiac disease or inflammatory bowel disease, can affect iron absorption. Effective management of these conditions is key to improving iron levels.