Prednisone often helps manage SLE symptoms; however, understanding its role and potential side effects is crucial. This article provides clear, concise information to help you work with your doctor for optimal management.
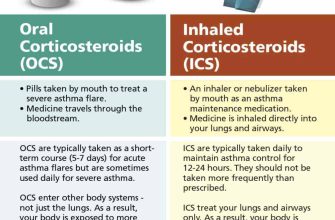
Remember, Prednisone is a powerful corticosteroid, not a cure. It primarily reduces inflammation, alleviating pain and fatigue associated with SLE flares. Expect improvements in joint pain, skin rashes, and other inflammatory symptoms. Your doctor will determine the appropriate dosage, and close monitoring is necessary.
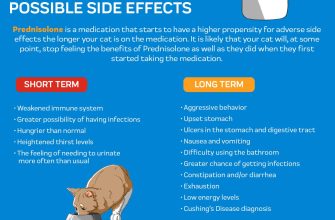
Potential side effects include weight gain, increased blood sugar, mood changes, and bone thinning. Open communication with your physician about any side effects is paramount. They can help adjust your medication or manage these issues. Regular blood tests monitor your response to treatment and detect potential complications.
Always follow your doctor’s instructions precisely. Self-adjusting your Prednisone dosage can be dangerous. Active participation in your treatment plan, including consistent medication adherence and attending follow-up appointments, ensures the best possible outcome. This proactive approach empowers you to manage SLE effectively and minimize long-term complications.
- Prednisone and SLE: A Detailed Overview
- Managing SLE with Prednisone
- Minimizing Prednisone Side Effects
- Alternative and Complementary Treatments
- Important Note:
- Understanding Prednisone’s Role in SLE Treatment
- Common Dosage and Administration of Prednisone for SLE
- Initial Treatment & Tapering
- Maintenance Therapy & Potential Adjustments
- Potential Side Effects of Prednisone in SLE Patients
- Common Side Effects
- Less Common, but Serious, Side Effects
- Managing Side Effects
- When to Contact Your Doctor
- Individualized Treatment
- Managing Prednisone Side Effects: Practical Tips
- Managing Mood Changes
- Addressing Other Side Effects
- Long-Term Prednisone Use and SLE Management: Considerations
- Tapering Off Prednisone: A Gradual Approach
Prednisone and SLE: A Detailed Overview
Prednisone, a corticosteroid, frequently treats Systemic Lupus Erythematosus (SLE) symptoms. It reduces inflammation and suppresses the immune system’s overactivity, a key factor in SLE’s pathogenesis.
Managing SLE with Prednisone
Doctors prescribe Prednisone for SLE flares, managing symptoms like joint pain, fatigue, and skin rashes. The dosage varies depending on severity; higher doses often address acute flares. Expect close monitoring for side effects.
- Dosage: Your rheumatologist determines the appropriate dose, adjusting it as needed based on your response and any side effects. Typical starting doses range from 5mg to 60mg daily, or even higher in severe cases.
- Duration: Treatment duration depends on your individual needs. Short-term use targets flares, while long-term use might be necessary for persistent symptoms. The goal is the lowest effective dose for the shortest duration.
- Side Effects: Common side effects include weight gain, increased appetite, fluid retention, mood changes, insomnia, increased blood sugar, and thinning bones (osteoporosis). Serious side effects, though less frequent, require immediate medical attention.
Minimizing Prednisone Side Effects
Several strategies help mitigate Prednisone’s side effects:
- Regular Monitoring: Frequent blood tests track your overall health and detect potential problems early.
- Lifestyle Adjustments: Maintain a healthy diet, exercise regularly, and prioritize sleep to support overall health and reduce side effect risks. Managing blood sugar and blood pressure are crucial.
- Medication Management: Your doctor may prescribe additional medications to counteract certain Prednisone side effects, such as medication for osteoporosis or high blood pressure.
- Gradual Tapering: Prednisone should be tapered off slowly, rather than abruptly stopped, to prevent a flare-up and minimize withdrawal symptoms. Never stop taking Prednisone without consulting your doctor.
Alternative and Complementary Treatments
While Prednisone is a cornerstone of SLE management, alternative and complementary therapies, like stress management techniques and physical therapy, can support overall well-being and improve quality of life. However, these should always be discussed with your doctor to ensure they don’t interfere with your Prednisone treatment.
Important Note:
This information provides a general overview. Always consult your physician or rheumatologist for personalized advice and treatment based on your specific health condition. Self-treating SLE with Prednisone or any medication is dangerous and can worsen the condition.
Understanding Prednisone’s Role in SLE Treatment
Prednisone, a corticosteroid, acts as a powerful anti-inflammatory drug, significantly reducing SLE symptoms. It targets the immune system, suppressing its overactivity which causes inflammation and damage in SLE. This leads to improvements in pain, fatigue, joint swelling, and skin rashes.
Doctors often prescribe prednisone for SLE flare-ups, providing rapid symptom relief. However, long-term use carries risks, including weight gain, osteoporosis, increased blood sugar, and increased susceptibility to infections. Your doctor will carefully monitor your condition and adjust your dosage accordingly.
The initial dosage varies depending on the severity of your SLE and response to treatment. Tapering off prednisone is crucial to minimize withdrawal symptoms and prevent relapse. This process usually involves gradually reducing the dose over several weeks or months under close medical supervision.
Prednisone isn’t a cure for SLE; it manages symptoms. It often works best in combination with other medications, like hydroxychloroquine or immunosuppressants, offering a more comprehensive approach to disease control. Open communication with your rheumatologist about your symptoms, side effects, and treatment goals is paramount.
Remember, regular checkups, including blood tests, are needed to monitor for side effects and ensure the prednisone dosage remains appropriate. Lifestyle modifications, such as regular exercise and a healthy diet, can also contribute to better management of SLE and minimize the impact of prednisone side effects.
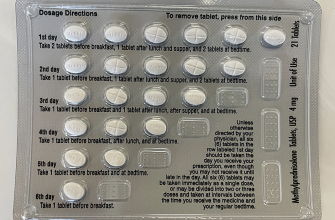
Common Dosage and Administration of Prednisone for SLE
Prednisone dosage for SLE varies greatly depending on disease severity and individual patient response. Your rheumatologist will determine the optimal dose and schedule. Initial dosages often range from 40-60 mg daily, gradually tapered down over several weeks or months. This tapering process is crucial to minimize side effects.
Initial Treatment & Tapering
High initial doses are common to achieve rapid disease control. However, prolonged high-dose prednisone carries significant risks. Doctors typically aim to reduce the dosage as quickly as possible while maintaining disease remission. The specific tapering schedule is individualized, based on your progress and tolerance of the medication. Regular monitoring of your SLE symptoms and potential side effects is necessary.
Maintenance Therapy & Potential Adjustments
Once a satisfactory response is achieved, the maintenance dose is often significantly lower, perhaps in the range of 5-10 mg daily or even less. This low dose helps prevent disease flares. However, your doctor may adjust the dosage based on ongoing assessment of your condition. Factors such as disease activity, side effects, and overall health will inform any adjustments. Remember, consistent communication with your healthcare provider is key.
Potential Side Effects of Prednisone in SLE Patients
Prednisone, while effective in managing SLE symptoms, carries potential side effects. Understanding these is key to managing your treatment effectively.
Common Side Effects
Many experience weight gain, increased appetite, and fluid retention. You might also notice mood changes, such as irritability or anxiety. High blood sugar is another possibility, so regular monitoring is recommended. Some patients report insomnia or increased blood pressure.
Less Common, but Serious, Side Effects
Less frequent, but requiring immediate medical attention, are serious side effects like osteoporosis (weakening of bones), cataracts, and glaucoma. Prednisone can also increase your risk of infections due to weakened immunity. Gastrointestinal problems, including ulcers and pancreatitis, are also possibilities.
Managing Side Effects
| Side Effect | Management Strategies |
|---|---|
| Weight gain | Maintain a healthy diet and regular exercise. Consult a nutritionist. |
| Mood changes | Maintain open communication with your doctor and consider counseling. |
| High blood sugar | Regular blood sugar monitoring and adjustments to medication or diet as needed. |
| Osteoporosis | Calcium and Vitamin D supplementation; discuss bone density testing with your physician. |
When to Contact Your Doctor
Report any concerning side effects immediately. This includes significant weight changes, persistent mood alterations, vision problems, severe stomach pain, or any signs of infection (fever, chills).
Individualized Treatment
Remember, your doctor will tailor your prednisone dosage and monitor you closely. Open communication is vital for managing your treatment and minimizing potential side effects.
Managing Prednisone Side Effects: Practical Tips
Track your weight daily. Weight gain is common; monitoring helps you catch it early and adjust your diet or discuss it with your doctor.
Eat a balanced diet rich in fruits, vegetables, and lean protein. This helps counter the effects of Prednisone on blood sugar and cholesterol.
Stay hydrated. Drink plenty of water throughout the day to help mitigate fluid retention.
Managing Mood Changes
Regular exercise can significantly improve mood swings associated with Prednisone. Aim for at least 30 minutes of moderate activity most days.
Prioritize sleep. Aim for 7-8 hours of quality sleep per night. Establish a relaxing bedtime routine to improve sleep quality.
Communicate with your doctor or therapist. Don’t hesitate to seek professional support if you experience persistent mood disturbances.
Addressing Other Side Effects
Use a gentle moisturizer to combat dry skin. Avoid harsh soaps and long, hot showers.
Take calcium and vitamin D supplements as prescribed by your doctor to protect bone health.
Monitor your blood pressure regularly. Prednisone can affect blood pressure; regular monitoring allows for timely adjustments.
Consult your doctor about any new or worsening symptoms. Open communication is key to effective management.
Long-Term Prednisone Use and SLE Management: Considerations
Minimize prednisone dosage as quickly as possible while maintaining disease control. Gradual tapering, guided by your rheumatologist, is key to preventing serious side effects.
Regular monitoring of blood pressure, blood glucose, and bone density is vital. These tests help detect and manage potential complications from prolonged prednisone use. Your doctor will schedule these appropriately.
Consider alternative therapies to reduce prednisone dependence. Biologics and other disease-modifying antirheumatic drugs (DMARDs) may help control SLE symptoms, allowing for lower prednisone doses.
Maintain a healthy lifestyle. Regular exercise, a balanced diet, and sufficient sleep support overall health and can positively impact SLE management. This includes maintaining healthy weight.
Address potential side effects proactively. Osteoporosis prevention strategies, such as weight-bearing exercises and calcium/vitamin D supplementation, are important. Manage high blood pressure and blood sugar levels diligently.
Open communication with your rheumatologist is paramount. Regular appointments allow for timely adjustments to your treatment plan and prompt addressing of any concerns. Discuss any new symptoms immediately.
Regular ophthalmological exams are recommended. Prednisone can cause cataracts and glaucoma, so early detection is crucial for treatment.
Explore support groups and resources for managing SLE and its associated challenges. Connecting with others facing similar situations can provide emotional support and practical advice.
Remember, long-term prednisone use requires a tailored approach. Work closely with your healthcare team to develop a personalized management strategy that balances disease control and minimizes risks.
Tapering Off Prednisone: A Gradual Approach
Never stop Prednisone abruptly. Your doctor will create a personalized tapering schedule, usually involving slow reductions in dosage over weeks or months. This prevents sudden withdrawal symptoms.
Expect potential side effects during tapering. These might include fatigue, muscle weakness, joint pain, and mood changes. Openly discuss these with your rheumatologist; they can help manage symptoms and adjust the tapering schedule accordingly.
Regular monitoring is key. Blood tests will track your SLE activity and help your doctor determine if the tapering pace is safe and effective. Schedule these appointments as your doctor recommends.
Consider lifestyle adjustments. A healthy diet, regular exercise (as tolerated), and stress management techniques can support your body during this process and improve your overall well-being. Sufficient sleep is also crucial.
Patient communication is paramount. Don’t hesitate to contact your doctor if you experience concerning symptoms or have any questions about the tapering process. Your health team is there to support you.
Remember, each individual’s experience with Prednisone tapering is unique. Your doctor’s guidance is fundamental to ensuring a safe and successful transition.