For moderate to severe COPD exacerbations, a typical prednisone dosage is 30-40mg daily for 5-7 days. This generally provides effective symptom relief. Remember, this is a guideline; your doctor will tailor the dosage to your specific needs based on your medical history and the severity of your symptoms.
Factors influencing the prednisone dose include the patient’s age, overall health, and the presence of other medical conditions. Higher doses might be considered in cases of severe exacerbations, but prolonged high-dose prednisone use carries risks of significant side effects. A gradual tapering of the dose after the initial course is usually recommended to minimize these risks.
Close monitoring of your response to treatment is critical. Report any worsening symptoms, such as increased shortness of breath or chest pain, to your physician immediately. They may adjust your medication or recommend additional therapies, such as bronchodilators or antibiotics, if necessary. Regular check-ups will also help track your progress and manage potential side effects. Always discuss any medication changes with your doctor before making adjustments to your treatment plan.
Important Note: This information is for general knowledge and does not constitute medical advice. Always consult with your healthcare provider for personalized guidance on managing your COPD and choosing the appropriate prednisone dosage for your situation. Ignoring medical advice could lead to serious complications.
- Prednisone Dose for COPD Exacerbation: A Comprehensive Guide
- Determining the Appropriate Prednisone Dosage
- Duration of Prednisone Treatment for COPD Flare-Ups
- Factors Influencing Treatment Length
- Potential Side Effects of Prednisone and Mitigation Strategies
- Gastrointestinal Issues
- Other Side Effects & Management
- Monitoring Response to Prednisone Treatment in COPD
- When to Consult a Doctor Regarding Prednisone Use for COPD
- Prednisone Side Effects Requiring Medical Attention
- Alternative Treatments and Adjunctive Therapies for COPD Exacerbation
Prednisone Dose for COPD Exacerbation: A Comprehensive Guide
The typical prednisone dose for a COPD exacerbation is 30-40 mg daily for 5-7 days. However, your doctor will determine the best dose for you based on your individual needs and the severity of your exacerbation.
Several factors influence the prescribed dosage:
- Severity of symptoms: More severe symptoms often require a higher initial dose.
- Patient response: Doctors may adjust the dose based on how well you respond to treatment. Improvement may warrant a gradual reduction.
- Patient characteristics: Age, weight, and other pre-existing conditions affect how your body processes prednisone.
- Comorbidities: Other health issues might influence dosing strategies.
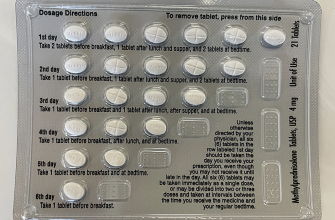
Common dosing regimens include:
- High-dose, short-course: This involves a high daily dose (e.g., 40mg) for a short period (e.g., 5 days), followed by tapering.
- Lower-dose, longer-course: A lower daily dose (e.g., 20mg) administered for a longer duration (e.g., 10-14 days), with a gradual reduction.
Important Considerations:
- Tapering: Abruptly stopping prednisone can lead to withdrawal symptoms. Your doctor will create a tapering schedule to reduce the dose gradually over several days or weeks.
- Side effects: Prednisone can cause various side effects, such as increased blood sugar, weight gain, insomnia, and mood changes. Discuss any concerns with your doctor.
- Alternative treatments: Prednisone is often used in conjunction with other treatments like bronchodilators and antibiotics.
- Regular monitoring: Your doctor will likely monitor your progress closely, adjusting the dose and treatment plan as needed.
This guide provides general information. Always follow your doctor’s instructions regarding prednisone dosage and treatment for your COPD exacerbation. They will personalize your care based on your specific medical history and current condition.
Determining the Appropriate Prednisone Dosage
The optimal Prednisone dosage for a COPD exacerbation depends on severity. A typical starting point is 30-40mg daily for 5-7 days.
Consider these factors for dose adjustment:
- Severity of symptoms: More severe shortness of breath, increased sputum production, or decreased oxygen saturation warrant a higher initial dose, potentially up to 60mg daily.
- Patient’s response: If symptoms significantly improve within a few days, consider tapering the dose. Lack of improvement suggests a need for reevaluation and potential dose increase (under medical supervision).
- Prior response to Prednisone: Patients who previously responded well to lower doses might benefit from a similar regimen, while those with poor responses might require a higher dose, again under physician guidance.
- Co-morbidities: Underlying conditions such as diabetes, heart failure, or osteoporosis can influence dosing and require careful monitoring.
Tapering is crucial to minimize side effects. A common strategy involves reducing the dose by 5-10mg every few days. Always follow your doctor’s instructions for tapering.
- Never abruptly stop Prednisone.
- Closely monitor for side effects such as increased blood sugar, insomnia, and fluid retention. Report any concerning symptoms immediately.
- Regular follow-up appointments are vital to assess treatment effectiveness and adjust the dosage as needed.
Remember: This information is for general knowledge only and does not replace professional medical advice. Always consult your physician or respiratory therapist for personalized treatment recommendations.
Duration of Prednisone Treatment for COPD Flare-Ups
Most guidelines recommend a short course of prednisone for COPD exacerbations, typically 5-7 days. This shorter duration minimizes potential side effects while effectively reducing inflammation and improving symptoms. A longer course isn’t usually necessary and may increase the risk of adverse events.
Factors Influencing Treatment Length
While 5-7 days is common, your doctor might adjust the duration based on your specific situation. Severe exacerbations might warrant a slightly longer course, perhaps up to 10-14 days, while milder cases may respond well to a shorter, 3-5 day treatment. Your response to the medication, the severity of your symptoms, and the presence of other health conditions will all play a role in determining the optimal treatment length.
Close monitoring of symptoms is vital. If your symptoms improve significantly within the initial days, your doctor may choose to shorten the course. Conversely, if your symptoms persist or worsen, they may extend it. Always follow your doctor’s instructions and contact them if you experience any concerning side effects or a lack of improvement.
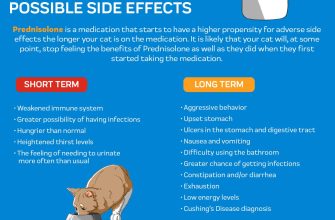
Potential Side Effects of Prednisone and Mitigation Strategies
Prednisone, while effective for COPD exacerbations, carries potential side effects. Increased blood sugar is common; monitor your blood glucose levels regularly, especially if you have diabetes. Consume smaller, more frequent meals to help manage this. Fluid retention can also occur, leading to swelling in your ankles and face. Reduce sodium intake and increase your water intake to counter this.
Gastrointestinal Issues
Prednisone can upset your stomach. Take it with food to minimize this. If you experience heartburn or indigestion, over-the-counter antacids may help. Severe stomach pain requires immediate medical attention. Increased risk of infections is another concern; practice good hygiene and avoid crowds when possible.
Other Side Effects & Management
Increased blood pressure is possible; regular monitoring is key. Your doctor might adjust your other medications accordingly. Mood changes, such as irritability or anxiety, may occur. Open communication with your doctor and loved ones is vital. Insomnia is another potential effect; maintain a consistent sleep schedule and avoid caffeine before bed. Muscle weakness and bone thinning are long-term risks; discuss potential countermeasures, like calcium supplements or weight-bearing exercise, with your physician. Always report any concerning symptoms to your doctor immediately.
Monitoring Response to Prednisone Treatment in COPD
Closely monitor your symptoms. Track your daily cough, sputum production (amount and color), and shortness of breath using a diary or app. Note any changes – improvement or worsening – and report them to your doctor.
Measure your peak expiratory flow (PEF) regularly. Aim for at least twice daily readings. Significant improvement should be seen within 24-72 hours. A lack of improvement or worsening PEF necessitates immediate medical attention.
Expect improved lung function within three to five days. If you don’t experience substantial symptom relief within this timeframe, contact your doctor. This is important to adjust your treatment plan.
Be aware of potential side effects. Prednisone can cause increased blood sugar, fluid retention, and insomnia. Report any concerning side effects to your physician promptly. Your doctor can manage these issues and adjust your treatment accordingly.
Follow your doctor’s instructions meticulously concerning tapering the prednisone dosage. Abrupt cessation can lead to serious complications. Always discuss any changes to your medication plan with your doctor.
Regular follow-up appointments are critical. These visits allow your doctor to assess your response to treatment and make necessary adjustments to your care plan. Schedule these appointments as advised by your healthcare provider.
When to Consult a Doctor Regarding Prednisone Use for COPD
Contact your doctor immediately if you experience any of the following while taking Prednisone for a COPD exacerbation: worsening shortness of breath, chest pain, increased heart rate, significant swelling in your legs or ankles, severe stomach pain, frequent or severe headaches, blurred vision, or unusual bruising or bleeding.
Prednisone Side Effects Requiring Medical Attention
Seek medical advice if you notice side effects such as mood changes (irritability, anxiety, or depression), insomnia, increased appetite with weight gain, or muscle weakness. These symptoms might require dosage adjustment or alternative treatment. Regular monitoring of blood sugar is vital if you have diabetes, as Prednisone can elevate blood glucose levels. Report any significant changes to your doctor.
Your doctor should also be consulted before stopping Prednisone; abrupt cessation can lead to serious complications. Always discuss your treatment plan and any concerns you have with your physician.
Alternative Treatments and Adjunctive Therapies for COPD Exacerbation
Consider pulmonary rehabilitation. This program improves breathing, strength, and endurance, reducing future exacerbations. A typical program involves exercise training, education on disease management, and psychosocial support.
Non-invasive ventilation (NIV) provides respiratory support without intubation. High-flow oxygen therapy can also improve oxygenation.
Antibiotics are crucial only if a bacterial infection is suspected. Your doctor will determine this based on symptoms and testing. Viral infections usually require supportive care.
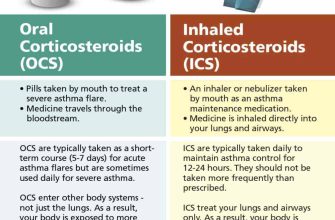
Bronchodilators, beyond what’s used for routine management, are frequently used during exacerbations. These medications relax airway muscles, easing breathing. Regular use of inhaled corticosteroids might also be recommended to reduce inflammation.
| Therapy | Mechanism of Action | Potential Benefits | Considerations |
|---|---|---|---|
| Roflumilast | Inhibits phosphodiesterase 4 | Reduces exacerbation frequency | Gastrointestinal side effects possible |
| Azithromycin (long-term low-dose) | Anti-inflammatory and antibacterial effects | May reduce exacerbation frequency | Potential for antibiotic resistance |
| Inhaled ipratropium bromide | Blocks muscarinic receptors | Reduces bronchoconstriction | May cause dry mouth |
Remember, treatment should be individualized. Your doctor will assess your specific needs and recommend the best approach for your condition. Discuss any concerns or questions with your healthcare provider.