For moderate asthma exacerbations, a typical starting dose is 40-60mg of prednisone daily. This usually provides significant relief within 24-48 hours. Remember to consult your doctor for personalized guidance.
Severe exacerbations may necessitate higher initial doses, potentially reaching 80mg daily. Your physician will carefully consider your specific needs and medical history to determine the most appropriate dosage.
Dosage adjustments are crucial. Your doctor will likely reduce the prednisone dose gradually once your symptoms improve to prevent rebound effects and minimize side effects. This tapering process is vital for preventing a relapse.
Important Note: This information serves as a general guideline only and does not substitute for professional medical advice. Always discuss your treatment plan with your doctor or other qualified healthcare provider. They can accurately assess your condition and prescribe the most suitable prednisone regimen for your unique circumstances, considering potential drug interactions and other health factors.
- Prednisone Dose for Asthma Exacerbation: A Detailed Guide
- Dosage Considerations
- Tapering Prednisone
- Understanding Asthma Exacerbations and their Severity
- Assessing Exacerbation Severity
- Categorizing Exacerbation Severity
- Impact of Severity on Prednisone Dosage
- Seeking Medical Advice
- The Role of Prednisone in Asthma Treatment
- Determining the Appropriate Prednisone Dosage
- Administration and Duration of Prednisone Treatment
- Monitoring Response to Prednisone Therapy
- Assessing Lung Function
- Monitoring Side Effects
- Potential Side Effects of Prednisone and Management Strategies
- Common Side Effects
- Less Common, but Serious Side Effects
- Alternative Treatments and Combination Therapies
- When to Seek Immediate Medical Attention
- Using Your Peak Flow Meter
- Severity Indicators
Prednisone Dose for Asthma Exacerbation: A Detailed Guide
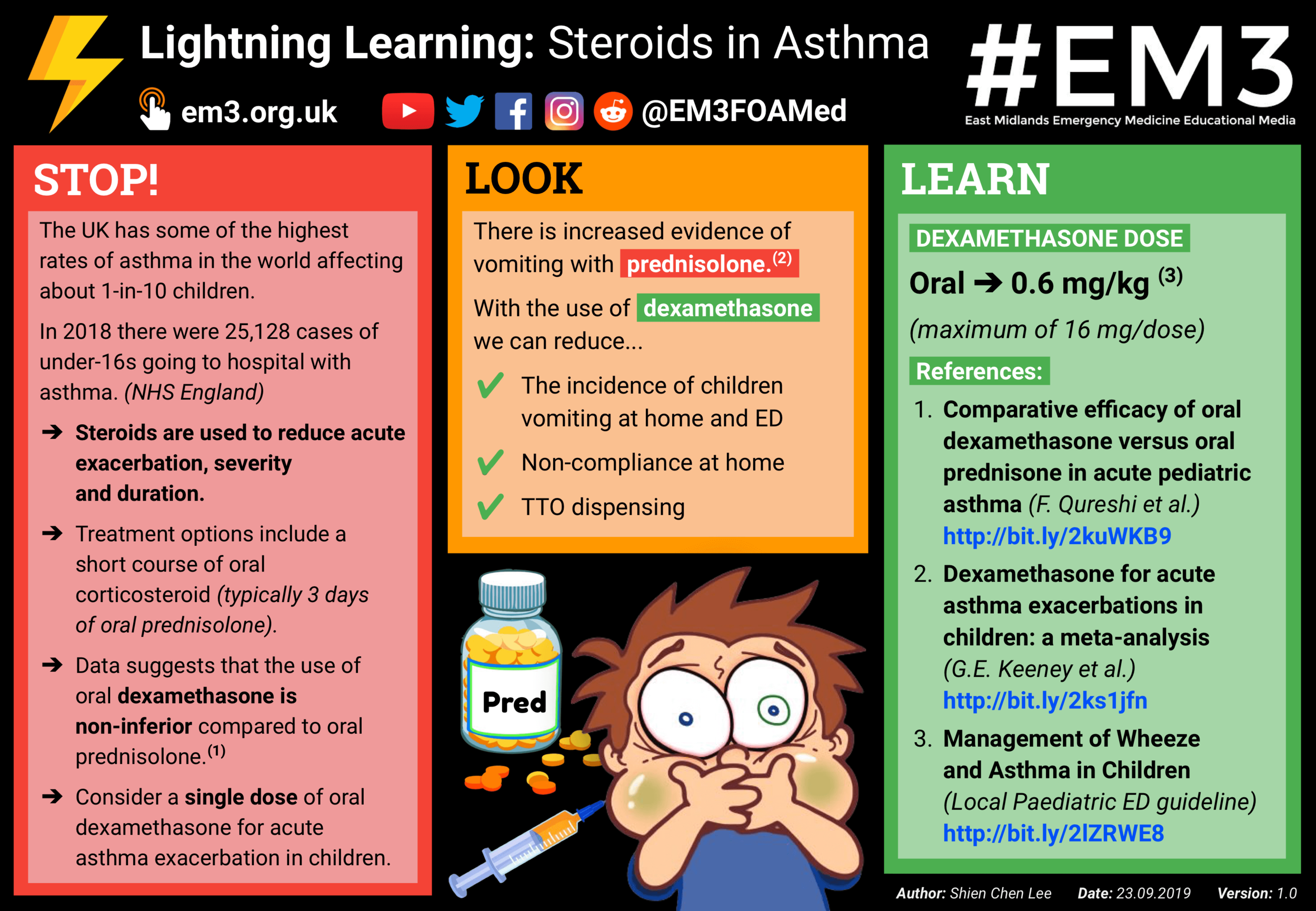
The typical initial prednisone dose for an adult with an asthma exacerbation requiring oral corticosteroids is 40-60 mg daily. Children receive a lower dose, calculated based on their weight. Always consult a physician for the appropriate dosage.
Dosage Considerations
Several factors influence the specific prednisone dose. These include:
- Severity of the exacerbation: More severe cases may require higher initial doses.
- Patient’s response to treatment: If symptoms don’t improve, adjustments may be necessary.
- Patient’s age and weight: Doses are adjusted based on these factors.
- Other medical conditions: Existing health issues could influence the dosage.
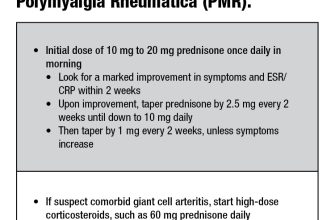
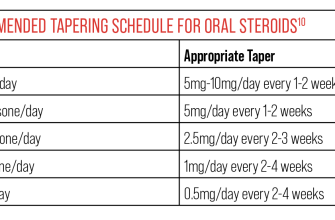
Treatment typically involves a short course of prednisone, usually lasting several days. A gradual tapering schedule is crucial to avoid withdrawal symptoms.
Tapering Prednisone
The physician will design a tapering schedule, often reducing the daily dose by a small amount every few days. A sample schedule (always follow your doctor’s instructions):
- Day 1-5: 60mg daily
- Day 6-8: 40mg daily
- Day 9-11: 20mg daily
- Day 12-14: 10mg daily
Abrupt cessation of prednisone can lead to relapse and other problems. Close monitoring by a healthcare professional is advisable throughout the treatment and tapering process. Remember to discuss any questions or concerns with your doctor. They will guide you through the best course of action for your specific situation.
Understanding Asthma Exacerbations and their Severity
Asthma exacerbations are worsening of asthma symptoms. Their severity varies greatly, impacting daily life differently for each person. Accurate assessment guides treatment decisions, including the appropriate prednisone dosage.
Assessing Exacerbation Severity
Doctors use several factors to determine severity. These include peak expiratory flow (PEF) readings, respiratory rate, oxygen saturation levels, and the patient’s overall condition. A low PEF, rapid breathing, low oxygen levels, and significant distress indicate a more serious exacerbation requiring stronger intervention.
Categorizing Exacerbation Severity
While categorization varies slightly between medical institutions, generally, exacerbations fall into mild, moderate, and severe categories. A mild exacerbation may only require adjustments to existing medication. A moderate exacerbation typically warrants a short course of oral corticosteroids like prednisone. Severe exacerbations necessitate immediate medical attention, often including hospitalization and potentially higher doses of corticosteroids, along with other treatments.
| Severity | PEF (% predicted) | Symptoms | Treatment |
|---|---|---|---|
| Mild | >80% | Minor increase in cough, wheezing, or shortness of breath | Increase in regular medication |
| Moderate | 50-80% | Increased cough, wheezing, shortness of breath, and some use of rescue inhaler | Short course of oral corticosteroids |
| Severe | <50% | Severe shortness of breath, rapid breathing, and reduced oxygen levels | Immediate medical attention, potentially hospitalization and higher doses of corticosteroids |
Impact of Severity on Prednisone Dosage
The severity of the exacerbation directly influences the prednisone dose prescribed. Mild exacerbations may not even require prednisone. Moderate cases typically benefit from a lower dose, while severe exacerbations may require significantly higher dosages to quickly control inflammation and improve breathing. Your doctor will determine the appropriate dosage based on your individual needs and the severity of your exacerbation.
Seeking Medical Advice
It is crucial to contact your doctor or seek immediate medical attention if you experience worsening asthma symptoms. They can accurately assess your condition and provide the most suitable treatment plan, including determining the correct prednisone dosage if needed.
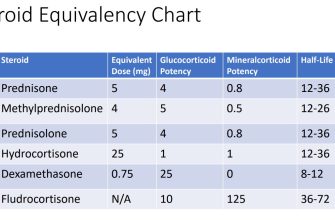
The Role of Prednisone in Asthma Treatment
Prednisone, a corticosteroid, acts swiftly to reduce airway inflammation, a key feature in asthma attacks. It’s not a long-term solution, but a powerful tool for managing exacerbations.
Here’s how it helps:
- Reduces swelling: Prednisone directly targets inflammation in the airways, decreasing swelling and making breathing easier.
- Decreases mucus production: It lessens the amount of mucus produced, opening up the airways further.
- Suppresses the immune response: This dampens the overactive immune response that triggers asthma symptoms.
Doctors prescribe prednisone for short-term use during asthma flares. The dosage and duration depend on the severity of your symptoms, typically ranging from a few days to a couple of weeks. Always follow your doctor’s instructions precisely.
While prednisone provides rapid relief, long-term use carries potential side effects, including:
- Weight gain
- Increased blood sugar
- High blood pressure
- Mood changes
- Weakened bones (osteoporosis)
Therefore, prednisone is best used as a short-term treatment for severe asthma episodes. It’s important to work with your doctor to manage your asthma long-term using inhalers and other preventative medications to minimize the need for prednisone.
Regular monitoring of your asthma, including peak flow measurements and adherence to your prescribed preventative medication plan, is key to preventing severe exacerbations and minimizing the need for steroid bursts.
- Discuss preventative strategies with your doctor.
- Understand your triggers and avoid them.
- Use your inhalers as directed.
- Seek medical attention promptly if your breathing worsens.
Determining the Appropriate Prednisone Dosage
For mild asthma exacerbations, a short course of 20-40mg of prednisone daily for 5-7 days often suffices. Adjustments depend on individual response.
Moderate exacerbations may require 40-60mg daily for 5-7 days. Close monitoring is vital. Consider longer duration if symptoms persist.
Severe exacerbations often necessitate higher doses, sometimes exceeding 60mg daily, potentially for a longer period, guided by clinical response and patient condition. Hospitalization may be necessary.
Children require pediatric dosing, adjusted for weight and severity. Always consult a pediatrician.
Factors influencing dosage include age, weight, disease severity, and response to treatment. Regular monitoring of lung function and clinical symptoms is crucial for optimal management.
Prednisone dosage is individualized; a physician will determine the most appropriate regimen based on your specific needs.
Never adjust your prednisone dosage without consulting your doctor. Sudden cessation can lead to rebound symptoms.
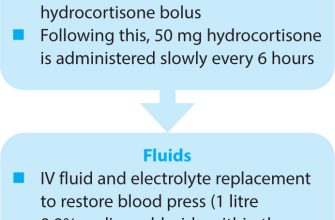
Administration and Duration of Prednisone Treatment
Prednisone for asthma exacerbation is typically administered orally, once daily, preferably in the morning. This timing helps minimize the potential for insomnia.
The recommended duration varies depending on the severity of the exacerbation and the patient’s response. For mild to moderate exacerbations, a 5- to 7-day course is often sufficient. More severe cases may require treatment for 10 to 14 days. Your doctor will determine the appropriate duration based on your individual needs.
Close monitoring of symptoms is vital. If symptoms improve significantly within a few days, your doctor might consider tapering the dose gradually towards the end of the treatment course to reduce the risk of side effects. However, abrupt cessation is generally avoided.
Always follow your doctor’s instructions regarding dosage and duration. Do not stop taking prednisone without consulting your doctor, even if you feel better. Stopping prematurely can lead to a relapse.
Remember to report any side effects to your doctor immediately. Common side effects include increased appetite, weight gain, mood changes, and increased blood sugar. Your physician can help manage these side effects.
Monitoring Response to Prednisone Therapy
Closely track your symptoms. Note any changes in your breathing, cough, wheezing, or chest tightness. Record your peak expiratory flow (PEF) readings regularly, ideally four times a day. Aim for at least a 15% improvement in your PEF from baseline within 24-72 hours. Lack of improvement warrants immediate medical attention.
Assessing Lung Function
Your doctor will likely assess your lung function through spirometry. Improvements in forced expiratory volume in 1 second (FEV1) and other parameters indicate a positive response. Expect significant improvements within a few days. Failure to show improvement after 72 hours necessitates a reassessment of your treatment plan.
Monitoring Side Effects
Prednisone can cause side effects. Watch for increased blood sugar, weight gain, mood changes, and insomnia. Report any significant side effects to your doctor immediately. Regular blood tests can help manage these effects. Open communication with your healthcare provider is paramount.
Potential Side Effects of Prednisone and Management Strategies
Prednisone, while effective for asthma exacerbations, can cause several side effects. Managing these is key to a positive treatment outcome.
Common Side Effects
- Increased appetite and weight gain: Monitor your diet and aim for a balanced nutritional intake. Regular exercise can help mitigate weight gain.
- Insomnia: Take your Prednisone dose earlier in the day. Avoid caffeine and alcohol before bed. Establish a consistent sleep schedule.
- Mood changes (irritability, anxiety, depression): Openly communicate with your doctor and family about how you feel. Consider stress-reducing techniques like meditation or yoga.
- Fluid retention (swelling): Reduce sodium intake in your diet. Your doctor can monitor this closely.
- Increased blood sugar: Regular blood sugar monitoring, particularly if you have diabetes, is necessary. Your doctor may adjust your diabetes medication.
- Gastrointestinal issues (heartburn, nausea, ulcers): Take Prednisone with food. Antacids may help with heartburn. Report persistent stomach pain to your doctor immediately.
Less Common, but Serious Side Effects
- Increased risk of infection: Practice good hygiene and avoid contact with sick individuals. Report any signs of infection to your doctor immediately.
- High blood pressure: Regular blood pressure monitoring is crucial. Your doctor might prescribe medication to manage it.
- Muscle weakness: Engage in gentle exercise, but avoid strenuous activity.
- Osteoporosis (long-term use): Discuss bone density monitoring with your doctor, especially if you are at increased risk. Calcium and Vitamin D supplementation may be recommended.
- Cushing’s syndrome (long-term high doses): This is a rare but serious complication. Your doctor will carefully monitor you for symptoms. Tapering off Prednisone gradually is crucial.
Remember, the duration of Prednisone treatment influences the likelihood of side effects. Always follow your doctor’s instructions regarding dosage and treatment duration. Open communication with your healthcare provider is paramount for managing potential side effects effectively and ensuring your asthma is managed safely.
Alternative Treatments and Combination Therapies
For milder asthma exacerbations, consider short-acting beta-agonists (SABAs) like albuterol for quick relief. Combine this with a short course of oral corticosteroids, like prednisone, to reduce inflammation. This combination often provides effective symptom control.
Inhaled corticosteroids (ICS) are a cornerstone of long-term asthma management. They reduce inflammation, preventing future exacerbations. Adding a long-acting beta-agonist (LABA) to your ICS can provide additional bronchodilation for better symptom control, especially during periods of increased asthma activity.
Biologic therapies, like omalizumab or mepolizumab, target specific inflammatory pathways. These are usually reserved for severe asthma that doesn’t respond well to standard treatments. Discuss these options with your doctor if other therapies prove inadequate.
Lifestyle modifications, including allergen avoidance, regular exercise, and smoking cessation, are crucial complements to medication. These measures can significantly improve asthma control and reduce the frequency of exacerbations.
Regular monitoring of peak expiratory flow (PEF) can help identify early signs of worsening asthma. This allows for timely intervention, potentially preventing a full-blown exacerbation and reducing the need for high-dose corticosteroids.
When to Seek Immediate Medical Attention
Go to the emergency room or call 911 immediately if you experience any of the following:
- Severe difficulty breathing or shortness of breath that doesn’t improve with your usual inhaler.
- Rapid breathing (more than 25 breaths per minute).
- Wheezing that’s loud enough to hear without a stethoscope.
- Blue discoloration of your lips or fingertips (cyanosis).
- Feeling unusually tired or weak.
- Confusion or disorientation.
- Chest pain or tightness.
These symptoms indicate a serious asthma exacerbation requiring urgent medical care. Don’t delay seeking help; early intervention can prevent life-threatening complications.
Using Your Peak Flow Meter
Regularly monitoring your peak expiratory flow (PEF) with a peak flow meter can help identify worsening asthma. A significant drop in your PEF readings (typically 50% or more below your personal best) signals a worsening condition and warrants immediate medical attention, regardless of other symptoms.
Severity Indicators
Use this table to assess your symptoms and decide if immediate medical attention is needed. Remember, this is a guideline, and your individual needs may vary.
| Symptom | Mild | Moderate | Severe (Seek Immediate Medical Attention) |
|---|---|---|---|
| Breathing Difficulty | Slight shortness of breath with exertion | Shortness of breath at rest, needs to sit up to breathe | Severe shortness of breath, cannot speak a full sentence |
| Wheezing | Occasional wheezing | Frequent wheezing | Loud, continuous wheezing |
| Cough | Mild cough | Persistent cough, producing sputum | Severe, unproductive cough |
| Activity Level | Mildly reduced activity | Significantly reduced activity | Unable to perform any activity |
Always consult your doctor or other healthcare professional for personalized advice on managing your asthma and when to seek medical attention. This information is not a substitute for professional medical advice.