Finding the right Prednisone dosage for rheumatoid arthritis (RA) is crucial for managing symptoms. Your doctor will personalize your treatment plan, typically starting with a higher dose to quickly reduce inflammation, often 7.5-60 mg daily. This initial phase aims for rapid symptom relief.
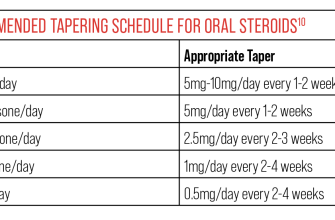
The dosage gradually decreases as your condition improves, a process known as tapering. Rapid tapering isn’t recommended as it can trigger a flare-up. Expect a slow, controlled reduction, often by 2.5-5 mg every few days or weeks, guided by your response and blood tests. Regular monitoring of blood pressure, blood sugar, and bone density is vital during treatment.
Important considerations include your overall health, other medications you’re taking, and your individual response to Prednisone. Some patients require lower doses for effective management, while others might need higher doses for a longer period. Side effects, such as weight gain, increased blood sugar, and mood changes, should be discussed with your doctor. They will help you manage these and adjust your treatment plan accordingly. The goal is to achieve optimal disease control with the lowest effective dose and minimize long-term side effects.
Remember, this information is for general knowledge and should not substitute advice from your rheumatologist or physician. They can assess your specific needs and determine the appropriate Prednisone dose and tapering schedule for you.
- Prednisone Dose for Rheumatoid Arthritis
- Starting and Tapering Prednisone Doses
- Starting the Medication
- Tapering Prednisone
- Monitoring for Side Effects
- Prednisone Dose Adjustments Based on Response
- Monitoring for Improvement
- Adjustments for Insufficient Response
- Managing Side Effects
- Common Side Effects and Management Strategies
- Gastrointestinal Issues
- Mood Changes and Sleep Disturbances
- Increased Blood Sugar and Blood Pressure
- Other Side Effects
- Long-Term Prednisone Use and Alternatives
Prednisone Dose for Rheumatoid Arthritis
Rheumatologists typically start Prednisone treatment for rheumatoid arthritis with a relatively high dose, often 7.5-60mg daily, to quickly control inflammation. This initial dose depends on disease severity and patient response. The goal is rapid symptom relief.
Dosage reduction begins once symptoms improve. This tapering process is gradual, usually involving decreases of 2.5-5mg every few days or weeks, under close medical supervision. Rapid tapering can lead to flares of the disease.
The target is the lowest dose that maintains symptom control. Many patients eventually reach a maintenance dose of 5mg or less daily, or even completely discontinue Prednisone after months or years. However, some may require ongoing low-dose Prednisone for long-term management.
Individual treatment plans vary. Factors influencing dosage include:
| Factor | Influence on Prednisone Dose |
|---|---|
| Disease severity | Higher initial doses for severe disease |
| Patient response | Dosage adjustments based on symptom improvement or worsening |
| Presence of other health conditions | Careful consideration of potential drug interactions |
| Age and overall health | Dosage adjustments may be needed for elderly or frail individuals |
Regular monitoring of blood pressure, blood sugar, and bone density is crucial during Prednisone treatment due to potential side effects. Close communication with your rheumatologist is absolutely necessary for safe and effective management of your rheumatoid arthritis.
Starting and Tapering Prednisone Doses
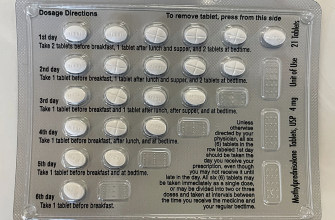
Your doctor will determine your starting Prednisone dose based on your specific needs and the severity of your rheumatoid arthritis. Common starting doses range from 5 to 60 mg daily, often in divided doses. Higher doses are usually used for short periods to control severe flares.
Starting the Medication
You’ll typically begin with a higher dose to quickly reduce inflammation. Follow your doctor’s instructions meticulously regarding frequency and timing of your doses. They may recommend taking the medication with food to minimize stomach upset. Regular blood tests will monitor your progress and ensure the medication is working effectively.
Tapering Prednisone
Once your inflammation is under control, your doctor will begin to gradually reduce your Prednisone dose. This tapering process is crucial to prevent withdrawal symptoms and relapse of your rheumatoid arthritis. Tapering is usually done in small increments, for example, decreasing by 2.5 mg every few days or weeks. The rate of tapering is individualized, depending on your response to treatment and the presence of side effects.
Monitoring for Side Effects
During both the starting and tapering phases, closely monitor yourself for side effects, such as weight gain, increased blood sugar, mood changes, and increased blood pressure. Report any concerns to your doctor immediately. They may adjust your dose or treatment plan accordingly. Remember, consistent communication with your healthcare provider is key to a safe and successful Prednisone treatment.
Prednisone Dose Adjustments Based on Response
Your doctor will carefully monitor your response to Prednisone. Initial doses often range from 5 to 60 mg daily, depending on disease severity. If your symptoms significantly improve within a few weeks, your doctor will likely begin tapering the dose, gradually reducing it by small increments (e.g., 5 mg every few days or weeks). This slow reduction minimizes the risk of withdrawal symptoms.
Monitoring for Improvement
Improvements are judged by assessing your symptoms such as joint pain, swelling, stiffness, and overall function. Blood tests monitoring inflammatory markers, like ESR and CRP, also play a crucial role in guiding dose adjustments. Significant improvement means less pain, better mobility, and decreased inflammation indicated by bloodwork.
Adjustments for Insufficient Response
If your symptoms don’t improve enough after a few weeks on a stable dose, your doctor might increase the Prednisone dosage. The increase will be carefully managed to balance symptom relief with potential side effects. Alternatively, they might add another medication to your treatment plan, such as a disease-modifying antirheumatic drug (DMARD), to work synergistically with Prednisone. This combined approach often leads to better outcomes.
Managing Side Effects
Dose adjustments also consider potential side effects. If side effects become bothersome, your doctor may reduce the dosage. They’ll weigh the benefits of Prednisone against the severity of the side effects. This balancing act requires careful monitoring and open communication between you and your doctor.
Common Side Effects and Management Strategies
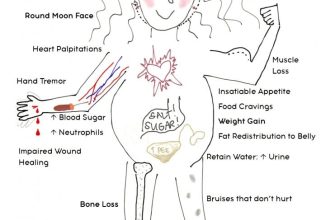
Prednisone, while effective for rheumatoid arthritis, can cause side effects. Weight gain is common; a balanced diet and regular exercise can help mitigate this. Increased appetite frequently accompanies this, so mindful eating habits are key.
Gastrointestinal Issues
Stomach upset, including heartburn and ulcers, is possible. Taking prednisone with food minimizes this risk. Your doctor might also prescribe a proton pump inhibitor to protect your stomach lining. Report persistent stomach pain immediately.
Mood Changes and Sleep Disturbances
Mood swings, anxiety, and insomnia are potential side effects. Maintaining a regular sleep schedule, reducing stress through relaxation techniques (like yoga or meditation), and discussing these changes with your doctor are helpful. They may recommend a low dose of an additional medication if needed.
Increased Blood Sugar and Blood Pressure
Prednisone can elevate blood sugar levels, increasing the risk of diabetes. Regular blood sugar monitoring is advised, alongside a diabetes-friendly diet if necessary. Similarly, blood pressure may rise; regular check-ups and lifestyle adjustments (diet, exercise) are crucial. Your doctor may prescribe medication to manage these.
Other Side Effects
Other possible side effects include increased risk of infection, thinning skin, easy bruising, and fluid retention. Maintaining good hygiene and avoiding contact with sick individuals helps prevent infection. Consult your doctor regarding any significant concerns.
Open communication with your rheumatologist is paramount for managing side effects. Don’t hesitate to report any new or worsening symptoms. They can adjust your dosage or prescribe additional medication to help you manage these effects and maximize the benefits of prednisone for your rheumatoid arthritis.
Long-Term Prednisone Use and Alternatives
Long-term prednisone use carries significant risks, including osteoporosis, cataracts, and increased risk of infections. Aim for the lowest effective dose and the shortest duration possible. Wean off slowly, under a rheumatologist’s supervision, to minimize withdrawal symptoms.
Consider these alternatives to long-term prednisone:
- Disease-Modifying Antirheumatic Drugs (DMARDs): Methotrexate, sulfasalazine, and leflunomide are cornerstone treatments, often reducing the need for high-dose steroids. Start these medications early in the disease course.
- Biologics: These targeted therapies, such as TNF inhibitors (e.g., adalimumab, etanercept) and IL-6 inhibitors (e.g., tocilizumab), effectively manage inflammation in many patients. Your doctor will determine which biologic is suitable for you based on your specific condition.
- Targeted Synthetic DMARDs (tsDMARDs): Janus kinase (JAK) inhibitors (e.g., tofacitinib, baricitinib) and other tsDMARDs offer additional options for those who don’t respond to or tolerate other treatments. These medications often work quickly, but side effects may include increased risk of infection.
Your doctor will create a personalized treatment plan based on your specific needs and response to therapy. Regular monitoring is crucial to track your progress, adjust medication as needed, and minimize potential side effects.
- Regular blood tests: Monitor blood counts, liver function, and kidney function.
- Bone density scans: Assess for osteoporosis risk, especially with prolonged prednisone use.
- Eye exams: Detect potential cataract development.
Open communication with your rheumatologist is key to successful management of rheumatoid arthritis. Don’t hesitate to ask questions and discuss any concerns you may have about your treatment plan.