Prednisone isn’t a first-line treatment for gout, but short-term use in a dose pack can provide significant pain relief. A typical course involves 6-day packs with varying doses, often starting higher and tapering down. Your doctor will determine the best dosage and duration for your specific needs, considering factors like your overall health and the severity of your gout attack.
Important Note: Prednisone’s anti-inflammatory effects target the symptoms of gout, not the underlying cause (uric acid buildup). While it rapidly reduces inflammation and pain, it doesn’t address the problem that leads to gout attacks. Therefore, combining prednisone with other medications, like allopurinol or colchicine, is frequently recommended to manage uric acid levels long-term and prevent future episodes.
Always consult your doctor before starting any medication, including prednisone. They can assess your condition, discuss potential side effects (such as increased blood sugar or stomach upset), and help create a personalized treatment plan. Self-treating gout can be harmful, so professional guidance is vital for effective management and preventing complications.
- Prednisone Dose Pack for Gout: A Detailed Guide
- What is Gout and How Does Prednisone Help?
- Standard Prednisone Dose Pack Regimen for Gout
- Important Considerations
- Alternative Regimens
- Potential Side Effects of Prednisone for Gout
- Common Side Effects
- Less Common but Important Side Effects
- Managing Side Effects
- Long-Term Use Considerations
- When to Consider Prednisone for Gout Treatment
- Alternatives to Prednisone for Gout Management
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
- Managing Prednisone Side Effects: Practical Tips
- Long-Term Gout Management Strategies Beyond Prednisone
- Lifestyle Modifications
- Medication
- Monitoring and Follow-up
Prednisone Dose Pack for Gout: A Detailed Guide
Prednisone, a corticosteroid, rapidly reduces inflammation associated with gout attacks. Doctors often prescribe a short course, typically a dose pack, to manage acute pain and swelling. This usually involves a decreasing dosage over several days.
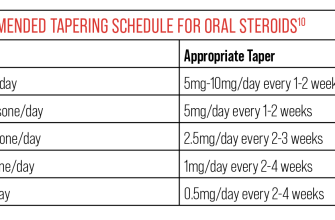
Typical Dosage Regimen: While specific dosages vary based on individual needs and doctor’s assessment, a common regimen involves a higher dose initially, followed by a gradual reduction.
- Day 1-2: High dose (e.g., 40mg)
- Day 3-4: Moderate dose (e.g., 30mg)
- Day 5-6: Lower dose (e.g., 20mg)
- Day 7: Lowest dose (e.g., 10mg)
This is just an example. Your doctor will determine the appropriate schedule for your specific situation.
Important Considerations:
- Side Effects: Prednisone can cause side effects, including increased appetite, weight gain, insomnia, mood changes, and increased blood sugar. These usually subside once you stop taking the medication.
- Long-Term Use: Prednisone is for short-term gout management. Long-term use carries significant risks.
- Other Medications: Inform your doctor about all medications you’re taking, including over-the-counter drugs, as interactions are possible.
- Underlying Conditions: Discuss any pre-existing health conditions with your doctor before starting Prednisone.
- Follow-up: Regular follow-up appointments are important to monitor your condition and treatment progress.
Remember: This information is for educational purposes only and does not replace professional medical advice. Always consult your doctor before starting any medication.
What is Gout and How Does Prednisone Help?
Gout is a form of arthritis caused by a buildup of uric acid crystals in your joints. This causes sudden, severe attacks of pain, swelling, redness, and tenderness, most often in your big toe.
Prednisone, a corticosteroid, helps by reducing inflammation. It doesn’t address the underlying uric acid problem, but it quickly tackles the painful symptoms of a gout attack.
- Prednisone works rapidly to decrease inflammation and pain.
- It’s typically prescribed as a short-term treatment for acute gout flares.
- A doctor usually prescribes a dose pack, meaning a pre-packaged course of medication to be taken over a few days.
While Prednisone offers swift relief, it’s crucial to remember it doesn’t cure gout. Long-term management involves lifestyle changes and possibly other medications to lower uric acid levels.
- Follow your doctor’s instructions precisely regarding dosage and duration.
- Discuss long-term gout management strategies with your doctor. This might include dietary changes, increased water intake, and medication to control uric acid levels.
- Report any side effects to your doctor immediately.
Prednisone provides significant short-term relief from gout symptoms, but it’s a part of a broader treatment plan, not a standalone solution.
Standard Prednisone Dose Pack Regimen for Gout
A typical prednisone dose pack for gout flare-ups involves a gradually decreasing dosage over several days. The most common regimen starts with 40mg on day one, followed by 30mg on day two, 20mg on day three, 10mg on day four, and 5mg on day five. After the fifth day, you’ll stop taking prednisone. This schedule provides rapid relief from inflammation and pain.
Important Considerations
Always follow your doctor’s instructions. This is a sample regimen, and your doctor may adjust it based on your specific needs and medical history. Do not exceed the prescribed dosage. Report any side effects to your doctor immediately. Prednisone can have side effects, and it’s not a long-term solution for gout. This treatment addresses the acute symptoms, not the underlying condition. Your doctor will likely discuss long-term management of your gout alongside this short-term treatment.
Alternative Regimens
While the 40mg-starting regimen is common, other dose packs exist. Your doctor might prescribe a lower starting dose or a different tapering schedule. They will make this determination based on factors such as your age, overall health, and the severity of your gout attack. Open communication with your physician is critical for successful treatment.
Potential Side Effects of Prednisone for Gout
Prednisone, while effective in reducing gout inflammation, carries potential side effects. These vary in severity and frequency, depending on the dosage and duration of treatment. Higher doses and longer treatment periods increase the risk.
Common Side Effects
Expect some common side effects, such as increased appetite leading to weight gain, fluid retention (causing swelling), and insomnia. You might also experience mood changes, ranging from mild irritability to anxiety. Some individuals report heartburn or indigestion.
Less Common but Important Side Effects
Less frequent, but still important to be aware of, are increased blood sugar levels (hyperglycemia), particularly concerning for those with diabetes. Prednisone can also increase blood pressure and elevate cholesterol levels. Muscle weakness and bone thinning (osteoporosis) are possible long-term risks with prolonged use. Rarely, but seriously, Prednisone can cause infections, so notify your doctor of any signs of infection.
Managing Side Effects
To minimize side effects, follow your doctor’s prescribed dosage and duration carefully. Maintain a healthy diet, prioritize regular exercise, and stay hydrated. Open communication with your physician is vital; report any concerning symptoms promptly. They may adjust your medication or suggest strategies to manage the side effects.
Long-Term Use Considerations
Long-term Prednisone use requires close monitoring by your doctor due to the increased risk of serious side effects. They will regularly assess your overall health and adjust your treatment plan accordingly. They may also prescribe additional medications to mitigate specific side effects.
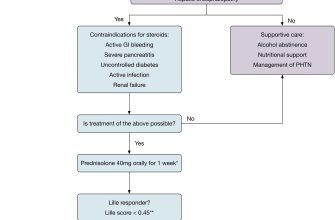
When to Consider Prednisone for Gout Treatment
Prednisone, a corticosteroid, offers rapid pain relief for gout flares, making it a valuable option when symptoms are severe. Consider it if your gout attack is intensely painful, significantly impacts your daily activities, or doesn’t respond adequately to NSAIDs.
However, remember Prednisone isn’t a first-line treatment. Your doctor will likely consider it if:
| Scenario | Why Prednisone Might Be Considered |
|---|---|
| Severe pain despite NSAIDs | Prednisone provides quicker, stronger anti-inflammatory action than NSAIDs. |
| Kidney or liver problems preventing NSAID use | Prednisone offers an alternative for patients with contraindications to NSAIDs. |
| Need for rapid symptom control | Prednisone’s rapid onset of action is beneficial for immediate pain relief. |
| Tophi (large uric acid deposits) causing significant discomfort | Prednisone can reduce inflammation around tophi, easing discomfort. |
A short course of Prednisone, usually a dose pack, often suffices. However, long-term use carries risks, so it’s crucial to discuss potential side effects and long-term gout management strategies with your physician. They will help create a plan that includes both acute flare management and long-term uric acid level control to prevent future attacks.
Alternatives to Prednisone for Gout Management
Colchicine remains a cornerstone of acute gout treatment. It effectively reduces inflammation and pain, often starting to work within hours. Your doctor will determine the appropriate dosage based on your individual needs and health status. Remember to inform your doctor about any other medications you’re taking to avoid potential interactions.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs like ibuprofen or naproxen provide effective pain relief and reduce inflammation. However, long-term use can carry risks, including stomach ulcers and kidney problems. Your physician can help you weigh the benefits against these potential risks and determine if NSAIDs are a suitable option for you. Always follow prescribed dosages.
For individuals who can’t tolerate NSAIDs or colchicine, your doctor might consider other options. These might include intra-articular corticosteroid injections directly into the affected joint, offering targeted relief. Another approach focuses on urate-lowering therapy (ULT). ULT medications, such as allopurinol or febuxostat, aim to decrease uric acid levels in the blood, preventing future gout attacks. Lifestyle changes, including dietary modifications and increased water intake, also play a crucial role in managing gout.
Managing Prednisone Side Effects: Practical Tips
Drink plenty of water throughout the day to stay hydrated. This helps your kidneys flush out the medication and reduces the risk of dehydration, a common side effect.
Eat small, frequent meals instead of three large ones. Prednisone can increase your appetite and lead to weight gain. Smaller portions help manage this.
Monitor your blood sugar levels regularly, especially if you have diabetes. Prednisone can elevate blood sugar.
Avoid alcohol. Alcohol interacts with prednisone, potentially increasing the risk of side effects like stomach upset.
Consider taking calcium and vitamin D supplements. Prednisone can increase calcium loss, leading to bone thinning.
Report any unusual bruising or bleeding to your doctor immediately. Prednisone can affect blood clotting.
Manage insomnia by creating a relaxing bedtime routine. Avoid caffeine and screen time before bed. If sleeplessness persists, talk to your doctor.
Keep track of your mood changes. Prednisone can sometimes cause mood swings or anxiety. Open communication with your doctor is key.
Use gentle skin cleansers and moisturizers. Prednisone can thin your skin, making it more prone to dryness and irritation.
Always follow your doctor’s instructions regarding dosage and duration of treatment. Don’t stop taking prednisone abruptly without consulting your physician.
Remember to contact your doctor if any side effects become severe or bothersome. They can offer tailored advice and adjust your treatment plan as needed.
Long-Term Gout Management Strategies Beyond Prednisone
Focus on a consistent, low-purine diet. Limit organ meats, red meat, shellfish, and sugary drinks. Increase your intake of fruits, vegetables, and whole grains. This dietary change significantly impacts uric acid levels.
Lifestyle Modifications
Maintain a healthy weight through regular exercise and a balanced diet. Weight loss, even modest, can substantially reduce gout flares. Aim for at least 150 minutes of moderate-intensity aerobic activity per week. Adequate hydration is key; drink plenty of water to help flush uric acid from your system. Quit smoking; it worsens gout.
Medication
Your doctor might prescribe urate-lowering therapy (ULT). Allopurinol is a common choice, helping your body excrete uric acid more efficiently. Febuxostat is another option. These medications are long-term and prevent future gout attacks. Discuss the potential side effects and monitoring requirements with your physician. Colchicine can help manage acute pain, but it’s not intended for long-term use.
Monitoring and Follow-up
Regular blood tests monitor your uric acid levels. These tests guide medication adjustments and track treatment success. Schedule regular check-ups with your doctor to discuss your progress and address any concerns. Understanding your triggers–foods, alcohol consumption, stress–helps you proactively manage the condition.