Prednisone can significantly reduce hand arthritis inflammation, providing pain relief. However, it’s a powerful medication, requiring careful management by your doctor. Expect to discuss your specific health situation, including other medications you’re taking, before starting Prednisone treatment.
Your physician will likely prescribe the lowest effective dose for the shortest duration possible. This minimizes the risk of side effects, such as weight gain, increased blood sugar, and increased blood pressure. Regular monitoring of your blood pressure and blood sugar levels will be necessary.
Don’t abruptly stop Prednisone; tapering the dose under medical supervision is crucial to prevent withdrawal symptoms. Your doctor will guide you through a safe tapering schedule, ensuring a smooth transition.
Alongside Prednisone, consider incorporating hand exercises recommended by a physical or occupational therapist. These exercises promote joint mobility and strength, complementing the medication’s anti-inflammatory effects. Remember, consistent exercise alongside medical treatment yields the best results.
Note: This information is for general knowledge only and doesn’t substitute professional medical advice. Always consult your doctor before starting or changing any medication regimen.
- Prednisone for Arthritis in Hands: A Comprehensive Guide
- Understanding Prednisone’s Role in Hand Arthritis Treatment
- Common Hand Arthritis Types Responsive to Prednisone
- Dosage and Administration of Prednisone for Hand Arthritis
- Oral Administration
- Duration of Treatment
- Important Considerations
- Monitoring Your Progress
- Alternative Treatments
- Disclaimer:
- Potential Side Effects and Managing Prednisone’s Risks
- Prednisone vs. Other Arthritis Medications for Hands
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- Disease-Modifying Antirheumatic Drugs (DMARDs)
- Biologics
- Choosing the Right Medication
- Long-Term Use and Tapering Off Prednisone
- When to Consult a Doctor About Prednisone for Hand Arthritis
- Side Effects Requiring Immediate Attention
- When to Discuss Dosage or Treatment Changes
Prednisone for Arthritis in Hands: A Comprehensive Guide
Prednisone, a corticosteroid, reduces inflammation and pain associated with hand arthritis. However, it’s not a long-term solution. Doctors typically prescribe it for short bursts to manage flare-ups.
Expect reduced swelling and improved hand mobility within days of starting treatment. Your doctor will determine the appropriate dosage and duration, usually a few weeks to a few months. They will carefully monitor your progress.
Common side effects include weight gain, increased appetite, mood changes, and difficulty sleeping. Less frequent but serious side effects can occur, such as increased blood sugar and weakening of bones. Report any concerning symptoms immediately to your physician.
Prednisone is often used in conjunction with other treatments like physical therapy and NSAIDs. Physical therapy helps maintain joint mobility and muscle strength. NSAIDs, like ibuprofen, provide additional pain relief and reduce inflammation.
Always inform your doctor about any other medications you’re taking, including over-the-counter drugs and supplements. This prevents potential interactions.
Gradually tapering off Prednisone, as directed by your physician, is crucial to minimize withdrawal symptoms. Sudden cessation can lead to a flare-up of arthritis symptoms.
| Dosage | Typical Duration | Potential Side Effects |
|---|---|---|
| Varies based on individual needs | Few weeks to a few months | Weight gain, increased appetite, mood changes, insomnia, increased blood sugar, bone weakening |
Prednisone offers temporary relief. Long-term management of hand arthritis often involves a combination of medication, therapy, and lifestyle adjustments. Consult your rheumatologist for a personalized treatment plan.
Understanding Prednisone’s Role in Hand Arthritis Treatment
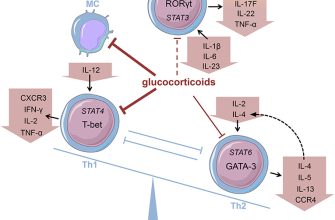
Prednisone, a corticosteroid, reduces inflammation in your hands, providing temporary pain relief and improved joint function. It’s often used for flare-ups of rheumatoid arthritis or osteoarthritis affecting the hands, offering quick symptom reduction.
Doctors typically prescribe prednisone for short periods, aiming to control symptoms until other treatments, like disease-modifying antirheumatic drugs (DMARDs), take effect. Long-term use carries risks like weakened bones and increased susceptibility to infections. Your doctor will carefully monitor your progress and adjust the dosage accordingly.
Prednisone comes in different forms, including tablets, and your doctor will determine the most appropriate dosage and treatment duration based on your specific condition and response. Always follow your doctor’s instructions precisely.
Potential side effects include weight gain, increased appetite, mood changes, and high blood sugar. Open communication with your doctor is crucial; report any unusual symptoms promptly. They may help manage side effects or adjust your treatment plan.
Prednisone isn’t a cure for hand arthritis; it manages symptoms. Combined with other therapies, like physical therapy and lifestyle modifications (diet and exercise), it can significantly improve your quality of life. Remember to discuss your treatment options thoroughly with your rheumatologist to create a personalized plan.
Common Hand Arthritis Types Responsive to Prednisone
Prednisone can effectively manage inflammation in several hand arthritis types. However, it’s crucial to remember it’s a short-term solution, not a cure.
- Rheumatoid Arthritis (RA): Prednisone reduces RA’s painful inflammation and swelling. It often provides rapid relief, but long-term use carries risks. Doctors usually prescribe it alongside disease-modifying antirheumatic drugs (DMARDs) for sustained management.
- Osteoarthritis (OA): While not directly addressing the cartilage degeneration underlying OA, prednisone can lessen the associated inflammation and pain in the hands. It’s frequently used for flare-ups, offering temporary relief.
- Psoriatic Arthritis: This inflammatory arthritis linked to psoriasis often responds well to prednisone’s anti-inflammatory effects. Similar to RA, it’s often a part of a broader treatment strategy to manage joint inflammation and prevent long-term damage.
- Gout: Prednisone can combat the intense inflammation characteristic of gout attacks. However, it’s not usually the first-line treatment; colchicine and NSAIDs are often preferred for acute gout. Prednisone may be used in severe cases or when other medications are ineffective.
Remember to discuss Prednisone use with your doctor. They will assess your specific condition, consider potential side effects, and create a personalized treatment plan.
- Your doctor will weigh the benefits against potential side effects, like weight gain, increased blood sugar, and weakened bones.
- They will monitor your progress closely while on Prednisone.
- A gradual tapering off of Prednisone is usually recommended to minimize withdrawal symptoms.
Dosage and Administration of Prednisone for Hand Arthritis
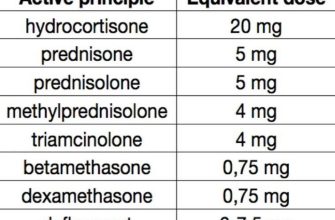
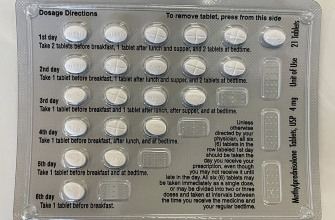
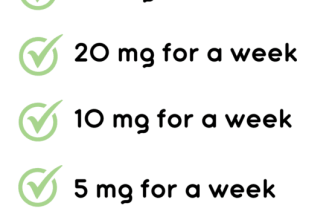
Your doctor will determine the appropriate prednisone dosage based on your specific condition and response to treatment. Typical starting doses range from 5 to 60 milligrams daily, often administered in divided doses. Higher doses are usually reserved for severe inflammation.
Oral Administration
Prednisone is typically taken orally, usually with food or milk, to minimize stomach upset. Follow your doctor’s instructions carefully regarding the frequency of administration (e.g., once daily, twice daily). Never adjust your dosage without consulting your physician.
Duration of Treatment
Prednisone is usually prescribed for short-term use due to potential side effects with prolonged use. Treatment duration varies depending on your individual needs and the severity of your hand arthritis. Your doctor will gradually reduce your dosage over time to minimize withdrawal symptoms.
Important Considerations
- Always inform your doctor about all medications you are taking, including over-the-counter drugs and supplements, as interactions may occur.
- Report any side effects to your doctor immediately, such as weight gain, increased appetite, mood changes, or fluid retention.
- Regular monitoring of blood pressure and blood sugar may be necessary, particularly with higher doses or longer treatment durations.
- Prednisone can weaken the immune system, increasing susceptibility to infections. Practice good hygiene and avoid contact with sick individuals.
Monitoring Your Progress
Regular appointments with your doctor are crucial to monitor your progress and adjust the dosage as needed. This ensures optimal pain management and minimizes potential side effects. Open communication with your doctor is key to successful treatment.
Alternative Treatments
Prednisone may be combined with other treatments like physical therapy or nonsteroidal anti-inflammatory drugs (NSAIDs). Your doctor will help determine the most effective treatment strategy for your particular situation. Discuss any concerns regarding alternative therapies with your physician.
Disclaimer:
This information is for educational purposes only and does not constitute medical advice. Always consult your physician for diagnosis and treatment of hand arthritis.
Potential Side Effects and Managing Prednisone’s Risks
Prednisone, while effective for hand arthritis, carries potential side effects. These vary by individual and dosage, but common ones include weight gain, increased appetite, fluid retention, mood changes (including irritability and anxiety), insomnia, and increased blood sugar.
To minimize risks, discuss your complete medical history with your doctor before starting Prednisone. This includes any existing conditions like diabetes or hypertension. Regular blood tests monitor potential side effects like elevated blood sugar and cholesterol.
Follow your doctor’s prescribed dosage carefully. Avoid abruptly stopping Prednisone; a gradual tapering off, as directed by your physician, is crucial to preventing withdrawal symptoms. Maintain a healthy diet and regular exercise to mitigate weight gain and improve overall health.
Report any unusual symptoms, such as severe headaches, blurred vision, or significant changes in mood, immediately to your doctor. Your doctor may also recommend dietary adjustments or additional medications to manage specific side effects.
Consider lifestyle modifications. Adequate sleep, stress management techniques (such as yoga or meditation), and a balanced diet can all contribute to better overall health and potentially lessen some side effects. Open communication with your physician is key to effectively managing your treatment and addressing any concerns.
Prednisone vs. Other Arthritis Medications for Hands
Prednisone offers rapid pain relief, making it a good initial treatment for severe arthritis flare-ups. However, it’s a corticosteroid with potential long-term side effects, so it’s usually not a long-term solution. Doctors often prescribe it for short bursts to manage symptoms until other medications take effect.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
NSAIDs like ibuprofen or naproxen provide pain relief and reduce inflammation. They’re available over-the-counter, but higher doses may require a prescription. While generally well-tolerated, long-term use can cause gastrointestinal problems. Consider combining NSAIDs with other therapies for optimal hand arthritis management.
Disease-Modifying Antirheumatic Drugs (DMARDs)
DMARDs, such as methotrexate or sulfasalazine, slow disease progression. They’re typically prescribed for longer-term management and are less effective at rapid pain relief than prednisone or NSAIDs. However, they offer a more sustainable approach to hand arthritis by targeting the underlying cause of the disease. Expect noticeable improvement to take weeks or months.
Biologics
Biologics are targeted therapies that interfere with specific parts of the immune system involved in arthritis. Examples include etanercept or adalimumab. They are highly effective for many, but may come with a higher risk of infection and other side effects. Your doctor will carefully weigh the benefits and risks based on your individual health.
Choosing the Right Medication
The best medication depends on your specific condition, its severity, your overall health, and other medications you’re taking. Open communication with your rheumatologist is key to developing a tailored treatment plan. Regular monitoring is crucial to assess the medication’s effectiveness and adjust the plan as needed. Don’t hesitate to discuss any concerns or side effects with your doctor.
Long-Term Use and Tapering Off Prednisone
Prednisone, while effective for managing arthritis pain, carries risks with prolonged use. Doctors generally avoid prescribing it for extended periods due to potential side effects like osteoporosis, high blood pressure, weight gain, and increased risk of infection.
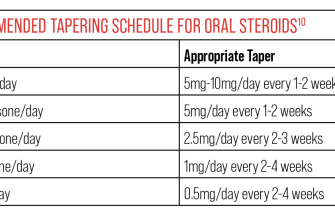
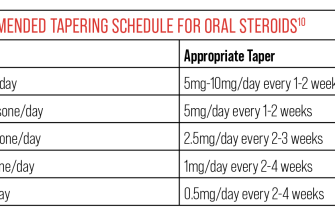
If you’ve been on prednisone for several weeks, discuss tapering with your doctor. Sudden cessation can trigger a flare-up of your arthritis symptoms and even cause adrenal insufficiency. A gradual reduction, following your doctor’s specific plan, is vital. This plan will usually involve decreasing your dose by a small amount at regular intervals – for example, by 5mg every few days or week.
Your doctor will monitor you closely during the tapering process, adjusting the schedule as needed based on your response. They may recommend blood tests to check your cortisol levels, ensuring your body can adequately produce its own steroid hormones.
Expect potential side effects during tapering, such as fatigue, joint pain, and muscle weakness. These are usually temporary and manageable. Maintain open communication with your rheumatologist – reporting any unusual symptoms immediately.
Remember, each individual responds differently to prednisone. Your doctor will create a personalized tapering plan tailored to your specific needs and health condition. Strict adherence to your doctor’s instructions is key to a successful and safe withdrawal from prednisone.
When to Consult a Doctor About Prednisone for Hand Arthritis
Schedule a doctor’s appointment if your hand arthritis pain doesn’t improve after two weeks of Prednisone, or worsens. Also, seek immediate medical attention if you experience any new or worsening side effects.
Side Effects Requiring Immediate Attention
Contact your doctor immediately if you experience significant weight gain, increased thirst or urination, blurred vision, easy bruising, mood changes (including irritability, anxiety, or depression), muscle weakness, or persistent nausea or vomiting. These could indicate serious complications.
When to Discuss Dosage or Treatment Changes
Discuss Prednisone dosage adjustments with your doctor if you experience significant side effects that are manageable but still impacting your quality of life. This includes less severe symptoms like indigestion, sleep disturbances, or mild acne. Your doctor can help determine if the benefits still outweigh the risks at your current dose, or if an alternative treatment plan is necessary.