Prednisone isn’t a first-line treatment for most childhood coughs. Doctors usually recommend trying other methods first, like rest, fluids, and over-the-counter medications. However, Prednisone can be helpful for specific types of coughs, particularly those related to allergies, asthma, or certain viral infections causing significant inflammation.
If your child’s cough is severe, persistent, or accompanied by wheezing, difficulty breathing, or fever, seek medical attention immediately. A doctor will assess your child’s symptoms and medical history to determine the underlying cause of the cough and decide if Prednisone is the appropriate treatment. This assessment will guide treatment decisions and avoid unnecessary medication.
Remember: Prednisone is a powerful steroid with potential side effects. Your doctor will carefully weigh the benefits against the risks before prescribing it. Closely follow the doctor’s instructions regarding dosage and duration of treatment. Report any unexpected side effects, such as increased thirst, frequent urination, or changes in mood or behavior, to your physician immediately. Never administer Prednisone without a doctor’s prescription.
This information is for educational purposes only and does not constitute medical advice. Always consult a pediatrician for diagnosis and treatment of your child’s cough.
- Prednisone for Cough in Kids: A Comprehensive Guide
- When is Prednisone Necessary?
- Understanding the Risks and Benefits
- Dosage and Administration
- Monitoring Your Child
- Alternative Treatments
- Prednisone vs. Other Treatments
- When to Seek Immediate Medical Attention
- When is Prednisone Considered for a Child’s Cough?
- Understanding the Risks and Benefits of Prednisone in Children
- Benefits
- Risks
- Important Considerations
- Dosage and Administration of Prednisone for Pediatric Coughs
- Oral Administration
- Duration of Treatment
- Important Considerations
- Common Side Effects of Prednisone in Children and How to Manage Them
- Behavioral Changes
- Physical Side Effects
- Important Note
- Alternative Treatments for Coughs in Children
- Saline Nasal Spray and Bulb Syringe
- Home Remedies
- When to See a Doctor
- When to Seek Immediate Medical Attention for a Child’s Cough
- Other Warning Signs
- When to Call Your Doctor Sooner Than Later
- Long-Term Effects and Follow-up Care After Prednisone Use
Prednisone for Cough in Kids: A Comprehensive Guide
Prednisone is a powerful corticosteroid, sometimes used to treat severe coughs in children caused by specific conditions, such as whooping cough (pertussis) or croup. It’s crucial to remember it’s not a first-line treatment for all coughs.
When is Prednisone Necessary?
Doctors typically prescribe Prednisone for coughs that are severe, persistent, and interfere with breathing or sleep. This usually involves a croupy cough or whooping cough. Viral infections often cause these, and Prednisone reduces inflammation, easing symptoms. However, it doesn’t treat the underlying virus itself.
Understanding the Risks and Benefits
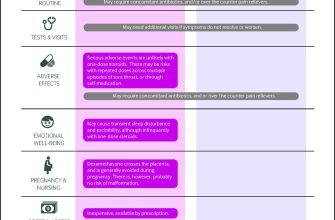
Prednisone offers rapid relief from inflammation. However, long-term use can have side effects, including increased risk of infection, weight gain, and mood changes. Therefore, it’s a short-term treatment, usually for a few days to a week, under strict medical supervision. A doctor assesses the benefit versus the risk for each child.
Dosage and Administration
Dosage depends on the child’s weight and the severity of the condition. A doctor will carefully determine the appropriate dose. Prednisone is usually given orally, as a liquid or tablet. Always follow the prescribed dosage exactly; never adjust it without consulting your doctor.
Monitoring Your Child
While your child takes Prednisone, closely monitor them for any adverse reactions, such as increased thirst, frequent urination, increased appetite, or mood changes. Report any concerns immediately to your doctor. Regular follow-up appointments are important to track progress and ensure the medication is working properly, and the potential side effects are being managed.
Alternative Treatments
Before considering Prednisone, many other treatments should be explored. These include supportive measures like rest, fluids, and over-the-counter medications like acetaminophen or ibuprofen to reduce fever and pain. A humidifier can also help soothe a cough.
Prednisone vs. Other Treatments
| Treatment | Use Cases | Advantages | Disadvantages |
|---|---|---|---|
| Prednisone | Severe croup, whooping cough | Rapid symptom relief | Potential side effects, not a cure |
| Humidifier | Most coughs | Soothes airways | May not be sufficient for severe cases |
| Rest and Fluids | Most coughs | Supports the body’s healing process | May not provide enough relief |
When to Seek Immediate Medical Attention
If your child experiences difficulty breathing, bluish discoloration of the skin, or persistent high fever, seek immediate medical attention. These can indicate serious complications. Always contact your doctor before giving your child any medication, including over-the-counter cough suppressants.
When is Prednisone Considered for a Child’s Cough?
Prednisone is usually reserved for coughs caused by croup, whooping cough (pertussis), or bronchitis that are severe enough to cause breathing difficulties. Doctors may consider it if a child has a persistent cough lasting longer than 10-14 days despite other treatments.
Specifically, prednisone might be used if a child experiences labored breathing, wheezing, or a barking cough (characteristic of croup). It can help reduce inflammation in the airways, alleviating these symptoms.
However, prednisone is not a first-line treatment for most coughs. Doctors typically try other methods, such as hydration, rest, and over-the-counter medications, first. The decision to prescribe prednisone will depend on the child’s age, overall health, and the severity of their cough and symptoms.
A doctor will assess the child’s condition thoroughly to determine if the benefits outweigh potential side effects before prescribing prednisone. Always follow your doctor’s instructions carefully.
Understanding the Risks and Benefits of Prednisone in Children
Prednisone can be a powerful tool for managing certain coughs in children, particularly those caused by inflammation, but it’s crucial to weigh the potential benefits against the risks.
Benefits
- Reduced inflammation: Prednisone significantly reduces swelling in the airways, easing breathing difficulties and suppressing a cough stemming from inflammation.
- Faster symptom relief: Many children experience quicker relief from cough and other symptoms compared to other treatments. This can improve their quality of life and allow for better rest.
- Improved sleep: A less severe cough allows for more restful sleep, which is particularly important for children’s growth and development.
Risks
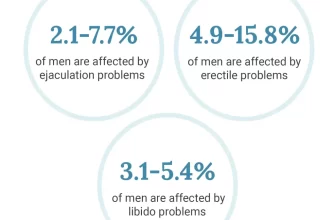
- Increased risk of infection: Prednisone suppresses the immune system, potentially making children more susceptible to infections like colds or flu.
- Side effects: Common side effects include increased appetite and weight gain, mood changes (irritability, anxiety), difficulty sleeping, and increased blood sugar. Rare but serious side effects can include cataracts, bone thinning, and increased blood pressure.
- Medication interactions: Prednisone can interact with other medications, so doctors need a complete medication history.
- Withdrawal effects: Abruptly stopping prednisone can lead to withdrawal symptoms, so tapering is usually necessary under a doctor’s supervision. This needs to be carefully managed.
Important Considerations
- Short-term use is generally preferred: Prednisone is most often prescribed for a short duration to manage acute symptoms. Prolonged use carries increased risk of side effects.
- Dosage is crucial: The doctor will determine the appropriate dose based on the child’s age, weight, and the severity of the condition.
- Close monitoring is necessary: Regular check-ups allow the doctor to monitor for side effects and adjust treatment as needed.
- Alternative treatments should be considered: In many cases, alternative treatments such as rest, fluids, and cough suppressants may be equally effective with fewer side effects.
Always discuss the risks and benefits of prednisone with your child’s doctor before starting treatment. They can help you make an informed decision that is best for your child’s health.
Dosage and Administration of Prednisone for Pediatric Coughs
Prednisone dosage for children with coughs depends heavily on the child’s weight and the severity of their condition. A doctor will always determine the appropriate dose. Typical pediatric dosages range from 1-2 mg per kilogram of body weight daily, administered in divided doses. For example, a 20 kg child might receive 20-40 mg per day, possibly split into two doses.
Oral Administration
Prednisone is usually given orally, meaning it’s swallowed as a tablet or liquid. Always follow your doctor’s instructions on how to administer the medication. For liquid forms, use the provided measuring device to ensure accuracy. Tablets can be crushed and mixed with food if necessary, but always check with the doctor or pharmacist first. Never exceed the prescribed dose.
Duration of Treatment
Prednisone treatment for coughs is typically short-term, usually lasting only a few days to a week. The doctor will adjust the duration based on the child’s response. Prolonged use can have side effects.
Important Considerations
Always inform your doctor about any other medications your child is taking. Some medications interact with prednisone. Monitor your child for side effects such as increased appetite, mood changes, or sleep disturbances. Report any concerning symptoms to your doctor immediately. Never stop prednisone abruptly; always follow the doctor’s tapering instructions to minimize withdrawal effects.
Common Side Effects of Prednisone in Children and How to Manage Them
Monitor your child closely for common side effects. Increased appetite and weight gain are frequent. Offer healthy, balanced meals and encourage physical activity to mitigate this. Increased thirst and frequent urination are also possible; ensure your child drinks plenty of water.
Behavioral Changes
Prednisone can sometimes cause mood swings, irritability, and difficulty sleeping. Maintain a consistent bedtime routine, create a calming bedtime environment, and speak to your pediatrician about potential adjustments to the medication schedule or dosage if sleep disturbances are severe. If your child exhibits unusual aggression or mood changes, consult your doctor immediately.
Physical Side Effects
Some children experience increased blood sugar levels. Regular blood sugar checks may be necessary, especially if your child has a family history of diabetes. Prednisone can also weaken the immune system, making your child more susceptible to infections. Practice good hygiene and avoid contact with sick individuals. If you notice any signs of infection, seek medical attention promptly. Finally, stomach upset is possible; smaller, more frequent meals can help.
Important Note
This information is for general knowledge and does not replace professional medical advice. Always follow your doctor’s instructions regarding Prednisone administration and management of side effects. Contact your pediatrician immediately if you have any concerns about your child’s health.
Alternative Treatments for Coughs in Children
First, consider increasing your child’s fluid intake. Warm liquids like broth or herbal tea (chamomile is often soothing) can help thin mucus and ease congestion. Offer plenty of water throughout the day.
Humidification is another helpful strategy. A cool-mist humidifier adds moisture to the air, which can soothe irritated airways and help loosen mucus. Ensure you clean your humidifier regularly to prevent mold growth.
Elevating your child’s head with extra pillows while sleeping can also provide relief. This helps drain mucus and makes breathing easier.
Saline Nasal Spray and Bulb Syringe
For children with nasal congestion contributing to their cough, a saline nasal spray or a bulb syringe can help clear their nasal passages. Gently squirt saline spray into each nostril or use the bulb syringe to suction out mucus. This can significantly reduce post-nasal drip.
Home Remedies
Honey (for children over 1 year old) can effectively suppress coughs. A teaspoon before bedtime can be quite helpful. You can also try a warm bath; the steam can help loosen chest congestion.
When to See a Doctor
While these alternative treatments can provide relief, it’s important to seek medical attention if your child experiences a high fever, difficulty breathing, persistent cough lasting more than two weeks, or a cough accompanied by wheezing. Early diagnosis is key.
| Treatment | Description | Age Recommendation |
|---|---|---|
| Increased Fluids | Water, broth, herbal tea | All ages |
| Humidifier | Cool-mist humidifier | All ages |
| Head Elevation | Extra pillows while sleeping | All ages |
| Saline Nasal Spray/Bulb Syringe | Clear nasal passages | All ages |
| Honey | One teaspoon before bed | Over 1 year old |
| Warm Bath | Soothes congestion | All ages |
When to Seek Immediate Medical Attention for a Child’s Cough
Contact your doctor or seek immediate medical attention if your child experiences any of the following:
- Difficulty breathing or rapid breathing: Noticeable shortness of breath, wheezing, or gasping for air requires immediate care.
- Bluish discoloration of lips or skin (cyanosis): This indicates a serious lack of oxygen and needs urgent medical attention.
- Severe retractions: If your child’s chest pulls in deeply with each breath (especially under the ribs or above the collarbone), seek immediate help.
- High fever (over 104°F or 40°C): A very high fever, especially combined with other symptoms, is a cause for concern.
- Persistent cough lasting more than three weeks: A prolonged cough warrants a doctor’s visit to rule out underlying conditions.
- Cough accompanied by a whooping sound: This suggests pertussis (whooping cough), which needs prompt treatment.
- Cough producing thick, discolored mucus: Yellowish-green or brownish mucus might indicate an infection requiring medical assessment.
- Dehydration: Signs include dry mouth, decreased urination, sunken eyes, or lethargy. Dehydration can be dangerous, especially in young children.
- Lethargy or unusual sleepiness: Significant changes in your child’s behavior, like excessive sleepiness or lack of responsiveness, should prompt a call to your doctor.
- Inability to drink or keep down fluids: This can lead to dehydration and requires medical attention.
Other Warning Signs
While not always requiring immediate emergency care, these symptoms warrant a prompt doctor’s visit:
- Persistent vomiting: Repeated vomiting can lead to dehydration and hinder recovery.
- Severe headache: A persistent or severe headache should be investigated.
- Stiff neck: This could be a sign of meningitis.
- Rash: A rash appearing alongside a cough needs evaluation by a doctor.
When to Call Your Doctor Sooner Than Later
- Your child is younger than 3 months old and has a cough.
- Your child’s cough worsens after initially improving.
- Your child is displaying symptoms that concern you, even if they aren’t listed above.
Remember, it’s always better to err on the side of caution. Trust your parental instincts, and don’t hesitate to contact your pediatrician if you have any concerns about your child’s cough.
Long-Term Effects and Follow-up Care After Prednisone Use
Schedule a follow-up appointment with your pediatrician to monitor your child’s progress after completing the Prednisone course. This allows for assessment of any lingering symptoms or side effects.
Weight gain is a common side effect. Monitor your child’s weight and discuss any significant changes with your doctor. Dietary adjustments might be necessary.
Increased appetite often accompanies Prednisone use. Healthy eating habits are crucial during and after treatment to prevent excessive weight gain.
Prednisone can temporarily increase blood sugar levels. Regular blood sugar checks may be recommended, especially if your child has a family history of diabetes.
Mood changes, including irritability or mood swings, can occur. Be patient and supportive; these typically subside after discontinuing Prednisone.
Weakened immune system is a potential concern. Avoid close contact with individuals who are sick to minimize the risk of infections. Discuss vaccination schedules with your pediatrician.
Slowed growth is a possibility with prolonged Prednisone use. Regular height and weight monitoring is recommended for children on long-term therapy.
If your child experiences any unexpected symptoms like severe abdominal pain, vomiting, or difficulty breathing, seek immediate medical attention. These could indicate serious complications.
Open communication with your pediatrician is key. Report any concerns or changes in your child’s health to ensure proper management and minimize potential long-term issues.