Finding the right Prednisone dosage for rheumatoid arthritis is crucial for managing symptoms. Your doctor will personalize your treatment based on your specific condition, including disease severity and overall health. They’ll likely start with a relatively low dose and carefully monitor your response.
Typical starting doses range from 5 to 60 milligrams daily, often decreasing gradually as your condition improves. This tapering process is key to minimizing side effects. Remember, abrupt cessation can lead to withdrawal symptoms. Close monitoring and consistent communication with your rheumatologist are vital throughout treatment.
Factors influencing dosage include age, weight, and response to therapy. Some patients may require higher doses initially, while others might find lower doses sufficient. Always follow your doctor’s instructions precisely, reporting any significant side effects immediately. Regular blood tests will monitor your progress and adjust the treatment plan accordingly.
Important Note: This information is for educational purposes only and should not replace consultation with a healthcare professional. Individual dosages vary significantly, and self-treating can be dangerous. Always seek guidance from your doctor or rheumatologist before starting or altering Prednisone treatment.
- Prednisone for Rheumatoid Arthritis Dosage: A Detailed Guide
- Dosage Adjustments
- Common Dosages & Schedules
- Potential Side Effects
- Alternatives and Combination Therapies
- Starting Dosage and Adjustment
- Dosage Reduction
- Factors Influencing Dosage
- Maintaining Low Dosage
- Monitoring for Side Effects
- Alternative Approaches
- Tapering Prednisone: A Safe Approach
- Slow and Steady Wins the Race
- Monitoring for Relapse
- Addressing Side Effects
- Alternative Medications
- The Importance of Patience
- Long-Term Management
- Prednisone Dosage Based on Disease Activity
- Common Side Effects and Dosage Considerations
- Prednisone and Other RA Medications
- When to Consult a Doctor Regarding Dosage
Prednisone for Rheumatoid Arthritis Dosage: A Detailed Guide
Your doctor will determine the appropriate Prednisone dosage for your specific needs, considering factors like your disease severity, overall health, and response to treatment. Initial doses often range from 5 to 60 milligrams daily, usually in divided doses. Higher doses are typically used for severe flares.
Dosage Adjustments
Your doctor will gradually reduce your Prednisone dosage once your symptoms improve. Rapid dose reductions can lead to a flare-up of your rheumatoid arthritis. Expect a slow tapering process, often over weeks or months, to minimize this risk. The exact tapering schedule depends on your individual circumstances.
Common Dosages & Schedules
While individual needs vary greatly, common Prednisone regimens might involve starting with a higher dose (e.g., 40mg daily) for several days, then gradually decreasing by 5-10mg every few days or weeks until reaching a maintenance dose or complete discontinuation. Some patients may remain on a low dose (e.g., 5-7.5mg) long-term. Always adhere to your physician’s prescribed schedule.
Potential Side Effects
Long-term Prednisone use carries risks, including weight gain, increased blood sugar, osteoporosis, and mood changes. Regular monitoring by your doctor is crucial to manage these potential side effects. Discuss any concerns you have with your healthcare provider immediately.
Alternatives and Combination Therapies
Prednisone often works best as part of a broader treatment plan, alongside disease-modifying antirheumatic drugs (DMARDs) or biologics. Your doctor might prescribe these medications to minimize Prednisone usage and reduce the risk of long-term side effects. Always discuss alternative treatments and their potential benefits and drawbacks with your doctor.
Starting Dosage and Adjustment
Prednisone treatment for rheumatoid arthritis usually begins with a relatively high dose, often 20-60 mg daily, to quickly reduce inflammation and pain. Your doctor will determine the optimal starting dose based on your specific condition and health. This initial phase is crucial for symptom control.
Dosage Reduction
Once your symptoms improve, your doctor will gradually reduce your prednisone dosage. This tapering process is vital to avoid sudden withdrawal symptoms and minimize the risk of side effects. The reduction rate varies depending on individual responses, usually occurring in small increments over weeks or months. For example, the dose might be decreased by 5 mg every few days or a week. Close monitoring by your doctor is essential during this phase.
Factors Influencing Dosage
Several factors influence the prednisone dosage and adjustment plan, including your disease severity, response to treatment, presence of other medical conditions, and tolerance to medication. Your doctor will carefully consider these aspects to create a personalized treatment plan. Regular blood tests may be necessary to monitor your progress and potential side effects.
Maintaining Low Dosage
The goal is to achieve remission or significantly reduce disease activity while minimizing the long-term effects of prednisone. Once a low maintenance dose is reached (often less than 10 mg daily or even less), your doctor will discuss strategies to further reduce or discontinue prednisone completely if possible, possibly alongside other therapies such as disease-modifying antirheumatic drugs (DMARDs).
Monitoring for Side Effects
Regular communication with your doctor is key. Report any new or worsening symptoms promptly. Common side effects of prednisone, such as weight gain, increased blood sugar, mood changes, and bone thinning, require close monitoring and may necessitate dosage adjustments or alternative treatments.
Alternative Approaches
If your condition doesn’t improve with prednisone, or if side effects are severe, your doctor may adjust your treatment plan. This may involve exploring alternative medications or therapies in conjunction with or instead of prednisone. Your doctor’s expertise and your own feedback are integral to successful rheumatoid arthritis management.
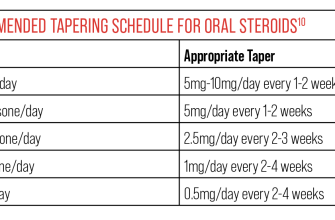
Tapering Prednisone: A Safe Approach
Always reduce your prednisone dose gradually, under your rheumatologist’s guidance. Never stop abruptly.
Slow and Steady Wins the Race
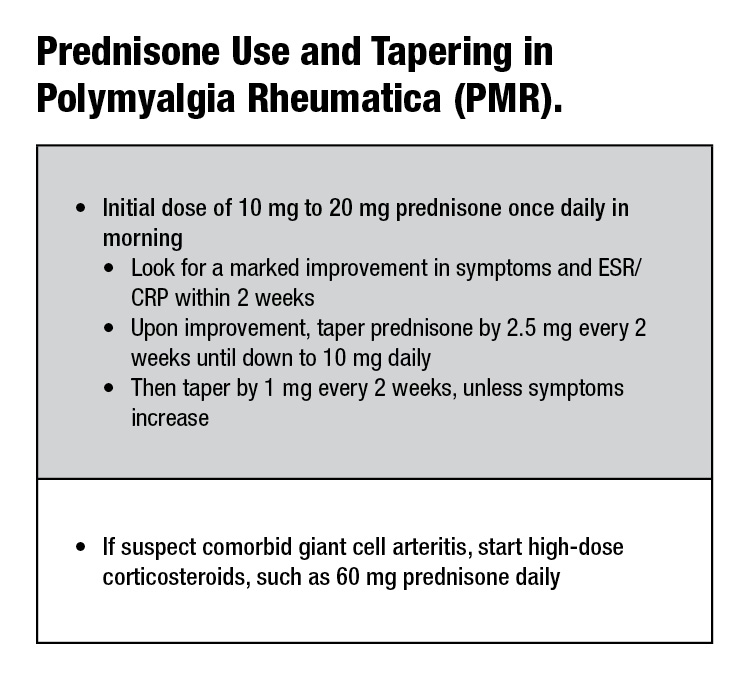
A typical tapering schedule might involve decreasing your dose by 5mg every 1-2 weeks. Your doctor will tailor this plan to your specific needs and response to treatment. Some individuals may require a slower reduction, perhaps 2.5mg every week or even less frequently. Factors influencing the tapering speed include your disease activity, overall health, and potential side effects.
Monitoring for Relapse
Closely monitor your rheumatoid arthritis symptoms throughout the tapering process. Report any worsening of joint pain, swelling, stiffness, or fatigue to your doctor immediately. Regular blood tests may be necessary to monitor your disease activity and ensure the tapering process is safe and effective.
Addressing Side Effects
Prednisone withdrawal can sometimes trigger side effects like fatigue, muscle weakness, and joint pain. Your doctor can help manage these symptoms and may adjust the tapering schedule if needed. Open communication with your rheumatologist is paramount.
Alternative Medications
Your doctor may introduce or increase other medications, such as disease-modifying antirheumatic drugs (DMARDs) or biologics, during the tapering period. This helps maintain control of your RA and minimizes the risk of a flare-up as prednisone is reduced.
The Importance of Patience
Tapering off prednisone takes time and patience. It is a process that requires close collaboration with your doctor. Your health and well-being are the priority. Do not rush the process.
Long-Term Management
After completing the tapering process, continue to work closely with your rheumatologist for ongoing management of your rheumatoid arthritis. Regular check-ups and proactive management will help ensure your long-term health and well-being. Maintain a healthy lifestyle including diet and exercise.
Prednisone Dosage Based on Disease Activity
Your doctor determines your Prednisone dosage based on your specific rheumatoid arthritis (RA) activity. This isn’t a one-size-fits-all approach. Higher doses are usually prescribed for severe, active RA, often starting at 40-60mg daily. This higher initial dose helps to quickly control inflammation and symptoms.
As your RA improves, your doctor will gradually reduce your Prednisone dosage. This tapering process is critical to prevent withdrawal symptoms and minimize side effects. The reduction rate varies depending on your response and individual needs. A common approach is to decrease the dose by 5-10mg every few days or weeks.
Maintaining a consistent medication schedule is paramount. Missing doses can disrupt treatment and exacerbate symptoms. Regular blood tests and clinical assessments will monitor disease activity and guide dosage adjustments.
Lower doses, perhaps 5-10mg daily, might be used for long-term management of RA in individuals with mild to moderate disease activity, alongside other disease-modifying antirheumatic drugs (DMARDs). However, long-term low-dose Prednisone can still pose risks.
| Disease Activity | Typical Starting Dosage (mg/day) | Tapering Strategy |
|---|---|---|
| Severe, Active RA | 40-60 | Gradual decrease by 5-10mg every few days/weeks |
| Moderate RA | 20-40 | Gradual decrease by 2.5-5mg every few days/weeks |
| Mild RA (often with DMARDs) | 5-10 | Careful monitoring, slow reduction as needed |
Remember: This table offers a general guideline. Your doctor will personalize your Prednisone regimen based on your individual health status, response to treatment, and potential side effects. Always communicate openly with your physician about any concerns or changes in your condition.
Common Side Effects and Dosage Considerations
Prednisone, while effective for rheumatoid arthritis, carries potential side effects. These depend on dosage and duration of treatment. Higher doses and longer treatment periods increase the risk.
Common side effects include weight gain, increased appetite, fluid retention (causing swelling), mood changes (including irritability and insomnia), high blood sugar, and increased risk of infections. Some individuals experience increased blood pressure or thinning of the bones (osteoporosis).
Dosage is highly individualized. Your doctor will determine the appropriate starting dose based on your specific condition and response to treatment. Typical starting doses range from 5 to 60 mg daily. The goal is to use the lowest effective dose for the shortest possible time. Your doctor will gradually reduce your dose once your symptoms improve, typically over weeks or months to minimize withdrawal symptoms.
Important note: Never abruptly stop taking prednisone. Sudden cessation can lead to serious complications. Always follow your doctor’s instructions regarding dosage reduction.
Monitoring is key: Regular check-ups allow your doctor to monitor your progress, assess side effects, and adjust your dosage accordingly. This may involve blood tests to check blood sugar, blood pressure, and other vital signs.
Lifestyle modifications can help manage side effects. A healthy diet, regular exercise, and stress management techniques can mitigate some of the negative impacts of prednisone.
Alternative therapies such as physical therapy and lifestyle changes can complement Prednisone treatment, and your doctor might suggest this approach to minimize the medication’s long-term use.
Consult your doctor immediately if you experience any unusual or concerning side effects. Open communication with your healthcare provider is crucial for safe and effective management of your rheumatoid arthritis.
Prednisone and Other RA Medications
Prednisone, while effective for managing rheumatoid arthritis (RA) flares, usually isn’t a long-term solution. Doctors typically prescribe it alongside other disease-modifying antirheumatic drugs (DMARDs) or biologics. This combination approach often provides better, more sustained RA control.
DMARDs, such as methotrexate, sulfasalazine, and hydroxychloroquine, slow disease progression. They are foundational treatments, often paired with Prednisone to rapidly reduce inflammation while the DMARDs take effect (this usually takes weeks or months). Prednisone helps manage symptoms during this crucial period.
Biologics, like TNF inhibitors (infliximab, adalimumab), are powerful medications targeting specific parts of the immune system. They’re reserved for moderate-to-severe RA cases unresponsive to DMARDs. Combining them with Prednisone, though less common than with DMARDs, can be beneficial during particularly aggressive flares or when switching between biologics.
Important Note: Always discuss medication combinations with your rheumatologist. They will tailor treatment to your specific needs, considering your RA severity, other health conditions, and potential drug interactions. Never stop or alter your medication regimen without consulting your doctor. Close monitoring is needed to ensure optimal outcomes and minimize side effects.
Your doctor might gradually reduce your Prednisone dose once your RA is under better control with other medications. This tapering process is vital to prevent withdrawal symptoms. Careful monitoring and adjustments are necessary throughout the treatment process.
When to Consult a Doctor Regarding Dosage
Contact your doctor immediately if you experience any of the following:
- Severe side effects, such as significant weight gain, fluid retention (edema), high blood pressure, or mood changes (irritability, anxiety, depression).
- Worsening of your rheumatoid arthritis symptoms despite taking Prednisone.
- Difficulty sleeping or insomnia.
- Increased appetite or cravings.
- Blurred vision.
- Increased susceptibility to infections.
- Bone pain or fragility.
- Muscle weakness or wasting.
- Increased blood sugar levels (especially if you have diabetes).
Schedule a consultation if you notice a gradual increase in any side effect, even if it seems minor. Regular monitoring is key for managing Prednisone treatment.
Always discuss any changes in your health status or medication with your physician before altering your Prednisone dosage. This includes changes to other medications you are taking. Your doctor will help you develop a safe and effective treatment plan.
Additionally, discuss your dosage plan with your physician if:
- You are planning pregnancy or are already pregnant.
- You’re considering breastfeeding.
- You are planning any surgery.
- You’re experiencing increased stress levels or changes in your lifestyle significantly impacting your health.
Regular communication with your doctor is paramount to ensure your Prednisone treatment remains safe and beneficial.