Prednisone can effectively reduce rhinitis symptoms, particularly inflammation. Doctors often prescribe it for severe allergic rhinitis or when other treatments fail. Remember, it’s a corticosteroid, so use it exactly as directed.
Expect relief from nasal congestion, sneezing, and itching within a day or two. However, Prednisone isn’t a long-term solution. Your doctor will likely recommend a tapering schedule to prevent withdrawal symptoms and minimize side effects. This gradual reduction is key for safe discontinuation.
Potential side effects include increased appetite, weight gain, mood changes, and insomnia. These usually subside once you stop the medication. Always inform your doctor about other medications you’re taking to avoid interactions. Regular monitoring of blood pressure and blood sugar might be necessary, especially for individuals with pre-existing conditions.
Alternative treatments, like antihistamines or nasal sprays, are often used alongside or instead of Prednisone for milder rhinitis cases. Discuss these options with your healthcare provider to create a personalized treatment plan that suits your specific needs and health history. They can assess your symptoms and determine the best course of action.
- Prednisone for Rhinitis: A Detailed Guide
- What is Rhinitis and When is Prednisone Necessary?
- Understanding Prednisone’s Role
- When to Consider Prednisone
- Understanding Prednisone: Mechanism of Action and Dosage for Rhinitis
- Dosage Considerations
- Potential Side Effects
- Potential Benefits and Limitations of Prednisone for Rhinitis
- Common Side Effects and Precautions When Using Prednisone
- Alternative Treatments for Rhinitis: Comparing Prednisone to Other Options
- Long-Term Use and Weaning Off Prednisone for Rhinitis
Prednisone for Rhinitis: A Detailed Guide
Prednisone, a corticosteroid, effectively reduces inflammation associated with severe allergic rhinitis. Doctors prescribe it for short-term relief of intense symptoms unresponsive to other treatments.
Typical dosage ranges from 20-60mg daily, adjusted based on individual needs and response. Your doctor determines the appropriate duration, usually 5-10 days. Longer use necessitates careful monitoring due to potential side effects.
Common side effects include increased appetite, weight gain, mood changes, insomnia, and increased blood sugar. Serious side effects are rare but include infections, glaucoma, and osteoporosis. Report any unusual symptoms immediately.
Prednisone isn’t a long-term solution. It addresses immediate inflammation; it does not treat the underlying cause of rhinitis. Your doctor will likely recommend additional strategies for long-term allergy management, such as allergy shots or antihistamines.
Never abruptly stop taking Prednisone. Gradual tapering, as directed by your physician, prevents withdrawal symptoms. Failure to follow this instruction can lead to a recurrence of rhinitis symptoms and other health issues.
This medication interacts with several other drugs. Inform your doctor of all medications, including over-the-counter remedies, you are taking to prevent adverse reactions. This includes herbal supplements and vitamins.
Consider using a nasal saline spray alongside Prednisone to help clear nasal passages and thin mucus. This can improve symptom relief. Always consult your doctor before using any medication.
Remember, this information is for educational purposes only and does not constitute medical advice. Always seek professional medical guidance for treatment of rhinitis or any health concern.
What is Rhinitis and When is Prednisone Necessary?
Rhinitis is inflammation of the nasal lining, causing symptoms like sneezing, runny nose, congestion, and itchy eyes. Allergic rhinitis stems from allergens like pollen or pet dander, while non-allergic rhinitis results from irritants or infections. Viral infections are the most common cause of non-allergic rhinitis.
Understanding Prednisone’s Role
Prednisone, a corticosteroid, powerfully reduces inflammation. Doctors prescribe it for severe rhinitis symptoms unresponsive to other treatments. This includes cases of allergic rhinitis causing significant breathing difficulties or persistent, debilitating symptoms. Non-allergic rhinitis might also warrant Prednisone if symptoms are intense and prolonged, especially if secondary bacterial infections develop.
When to Consider Prednisone
Consider Prednisone if: your rhinitis symptoms severely impact your daily life, including sleep and work; over-the-counter medications provide insufficient relief; you experience significant nasal congestion obstructing breathing; you suspect a secondary bacterial infection complicating your rhinitis.
Important Note: Prednisone is a powerful medication with potential side effects. Only a doctor can determine if it’s the right treatment for you. They will weigh the benefits against potential risks, considering your overall health and medical history. Always discuss treatment options with your physician before starting any medication.
Understanding Prednisone: Mechanism of Action and Dosage for Rhinitis
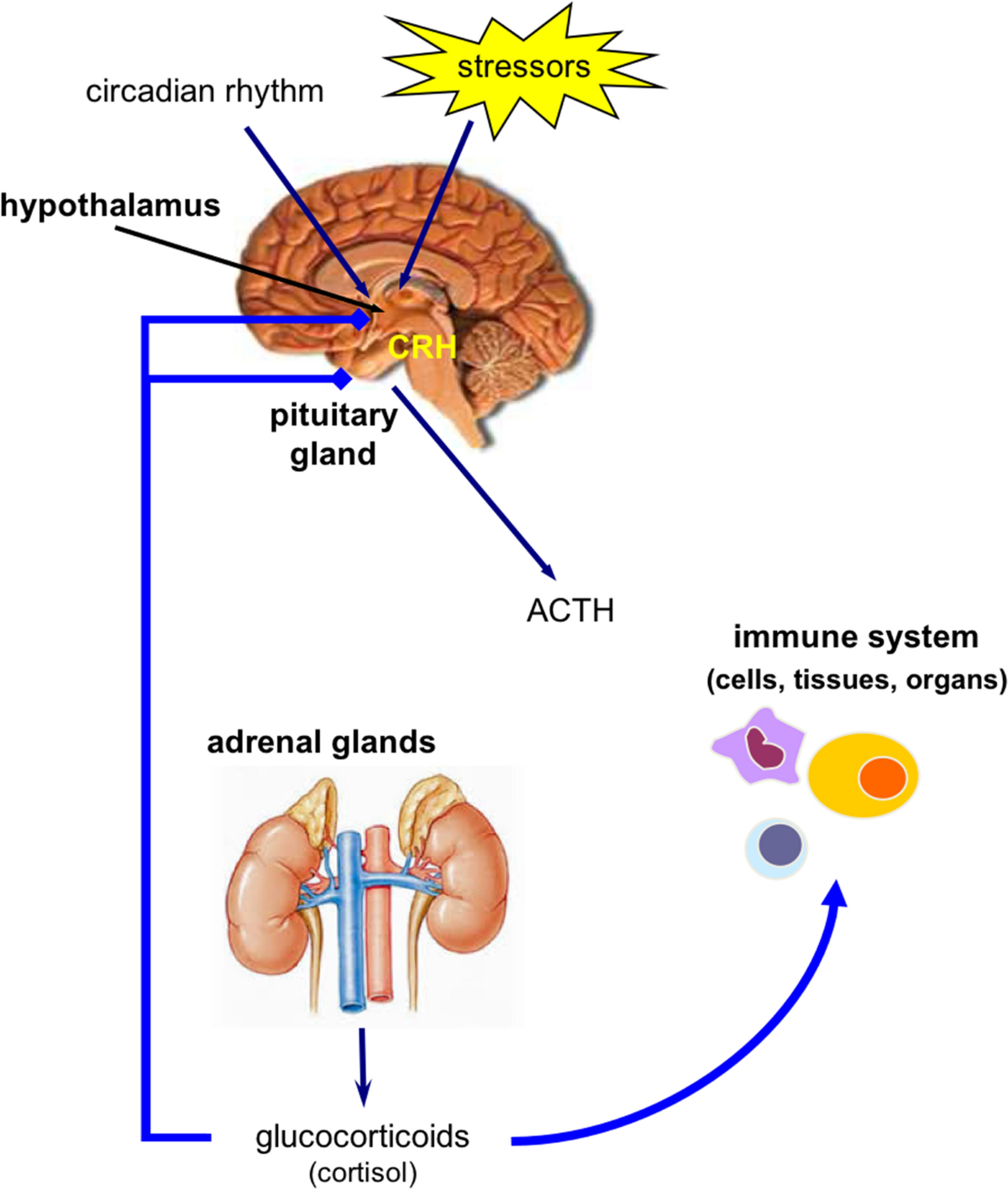
Prednisone, a corticosteroid, reduces rhinitis symptoms by suppressing inflammation. It achieves this by binding to glucocorticoid receptors within immune cells, hindering the release of inflammatory mediators like histamine and leukotrienes. This, in turn, lessens nasal congestion, sneezing, and itching.
Dosage Considerations
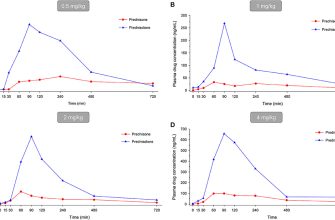
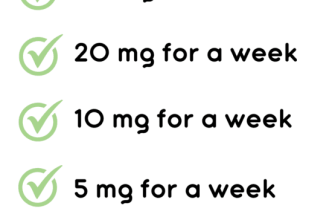
The prescribed prednisone dosage for rhinitis varies depending on the severity of your symptoms and your individual health profile. Typically, doctors recommend a short course of medication, usually lasting a few days to a week. Common dosages range from 5mg to 60mg daily, often taken in a single dose in the morning. Always adhere to your doctor’s instructions precisely. Higher dosages may be necessary for severe cases, but prolonged use carries potential side effects, so careful monitoring by your healthcare provider is vital. Never adjust your dosage without consulting your physician.
Potential Side Effects
While prednisone effectively alleviates rhinitis symptoms, potential side effects include increased appetite, weight gain, mood changes, insomnia, and increased blood sugar. These side effects are usually mild and temporary, especially with short-term use. Inform your doctor immediately about any concerning symptoms. The benefits of prednisone for treating severe rhinitis usually outweigh the risks of short-term use, when prescribed and managed correctly.
Potential Benefits and Limitations of Prednisone for Rhinitis
Prednisone offers rapid relief from severe rhinitis symptoms. It powerfully reduces inflammation, quickly alleviating nasal congestion, sneezing, and itching. This makes it particularly useful for managing acute flare-ups or allergic reactions causing significant distress.
However, Prednisone isn’t a long-term solution. Prolonged use carries risks, including increased blood sugar, weakened immunity, and bone thinning. Doctors generally prescribe it for short courses, focusing on symptom control during intense periods of rhinitis.
Furthermore, Prednisone’s powerful effects can mask underlying conditions, delaying proper diagnosis. Additionally, it may cause side effects such as insomnia, increased appetite, and mood changes in some patients. A doctor should carefully weigh benefits against potential side effects for each individual.
Consider alternatives like intranasal corticosteroids for longer-term management of chronic rhinitis. These medications offer similar anti-inflammatory benefits with a lower risk of systemic side effects. Always consult a healthcare professional to determine the best treatment plan for your specific situation.
Common Side Effects and Precautions When Using Prednisone
Prednisone, while effective for alleviating rhinitis symptoms, can cause side effects. Common ones include increased appetite, weight gain, fluid retention, and mood changes like irritability or anxiety. Some individuals experience insomnia or difficulty sleeping.
More serious, though less frequent, side effects include increased blood sugar levels, potentially worsening existing diabetes, and increased risk of infection. High blood pressure is also a possibility.
To minimize risks, discuss your complete medical history with your doctor before starting Prednisone. This includes existing conditions like diabetes, hypertension, or glaucoma. Inform your physician about all medications you are currently taking, including over-the-counter drugs and supplements, to avoid potential interactions.
Follow your doctor’s prescribed dosage carefully and do not abruptly stop taking Prednisone, even if you feel better. Sudden cessation can lead to withdrawal symptoms. Your doctor will help you gradually reduce your dosage as needed.
Monitor your blood sugar levels regularly if you have diabetes. Regular check-ups with your doctor are crucial to monitor for any potential side effects and adjust treatment accordingly. Report any unusual symptoms immediately.
Remember, Prednisone is a powerful medication. Proper usage and careful monitoring are key to maximizing its benefits and minimizing potential risks.
Alternative Treatments for Rhinitis: Comparing Prednisone to Other Options
Prednisone provides quick relief, but it’s a steroid with potential side effects. Let’s explore better alternatives.
- Intranasal corticosteroids: These are your first line of defense against allergic rhinitis. Brands like fluticasone (Flonase) and mometasone (Nasonex) reduce inflammation directly in the nasal passages, minimizing systemic side effects compared to oral steroids like prednisone. Expect symptom relief within a few days, but consistent daily use is key for ongoing management.
- Antihistamines: Cetirizine (Zyrtec), fexofenadine (Allegra), and loratadine (Claritin) effectively combat allergy symptoms like sneezing, itching, and runny nose. They’re available over-the-counter and generally well-tolerated, though drowsiness can occur with some. Consider non-drowsy options if you need to drive or focus.
- Decongestants: Pseudoephedrine (Sudafed) and phenylephrine constrict blood vessels in the nasal passages, providing temporary relief from stuffiness. However, prolonged use can lead to rebound congestion, so use them sparingly and as directed. Avoid combining decongestants with other medications without consulting your doctor.
- Saline nasal sprays: These are gentle and safe for daily use. They help rinse out allergens and irritants, providing immediate relief from stuffiness and dryness. Look for isotonic solutions – these match the salt concentration of your nasal passages.
- Allergen immunotherapy (allergy shots): This is a long-term approach that gradually desensitizes your immune system to specific allergens. It’s not a quick fix, requiring several months or even years of treatment, but it can provide lasting relief and reduce reliance on other medications. Consult an allergist to determine suitability.
Choosing the right treatment depends on several factors:
- Severity of symptoms: Mild symptoms might respond well to antihistamines or saline sprays. More severe cases may necessitate intranasal corticosteroids or a combination approach.
- Underlying cause: Allergic rhinitis requires a different approach than non-allergic rhinitis. Identifying the trigger is crucial for successful treatment.
- Individual tolerance: Some people experience side effects from certain medications. Discuss potential side effects and alternatives with your doctor.
Remember to consult your doctor or allergist before starting any new treatment, especially if you have pre-existing conditions or are taking other medications. They can help you create a personalized plan for managing your rhinitis effectively and safely.
Long-Term Use and Weaning Off Prednisone for Rhinitis
Prednisone shouldn’t be a long-term solution for rhinitis. Extended use increases the risk of side effects like weight gain, high blood pressure, and bone thinning. Always aim for the shortest duration possible to control symptoms.
Your doctor will create a tapering schedule. This means gradually reducing your prednisone dosage over several weeks or months. Never stop abruptly.
| Step | Action | Potential Side Effects (Consult your doctor immediately if experienced) |
|---|---|---|
| 1 | Reduce dosage by a small amount (as prescribed by your doctor). | Increased inflammation, fatigue, joint pain. |
| 2 | Monitor for symptoms. If symptoms worsen, temporarily maintain the dosage before resuming reduction. | Increased inflammation, fatigue, joint pain. |
| 3 | Continue decreasing the dosage following your doctor’s plan. | Symptoms may fluctuate; fatigue and sleep disturbances are common. |
| 4 | Regularly check your blood pressure and weight. | Blood pressure changes, weight fluctuations. |
During weaning, consider alternative treatments like nasal corticosteroids or antihistamines to manage rhinitis symptoms. These medications can help minimize the need for prednisone and provide more sustained symptom relief. Your doctor can help you determine the best combination of treatments.
Regular follow-up appointments are critical for monitoring progress, adjusting the weaning schedule, and managing any potential side effects. Open communication with your healthcare provider is essential for successful weaning and managing your rhinitis effectively.