Don’t prolong Prednisone use without close medical supervision. Your doctor should carefully monitor your health and adjust your dosage gradually to minimize withdrawal symptoms and long-term side effects. This includes regular blood tests to check for potential complications.
Prolonged Prednisone use significantly increases your risk of osteoporosis, cataracts, and infections. To mitigate this, your physician may prescribe calcium and vitamin D supplements, along with strategies to prevent falls and manage infection risks. Open communication with your healthcare provider is paramount.
Consider alternative treatment options if possible. Your doctor might explore less potent steroids or other medications to address your underlying condition. This collaborative approach prioritizes your well-being and minimizes dependence on Prednisone.
Regular exercise and a balanced diet are crucial for maintaining overall health, especially during prolonged Prednisone use. These lifestyle adjustments can help offset some of the medication’s negative impacts. Consult a dietitian or physical therapist for personalized guidance.
- Prednisone Long Term: A Detailed Guide
- Managing Side Effects
- Tapering Off Prednisone
- Alternative Treatments
- Monitoring Your Health
- Lifestyle Adjustments
- Long-Term Prednisone and Mental Health
- Understanding the Risks of Long-Term Prednisone Use
- Managing Prednisone Side Effects: A Practical Approach
- Monitoring Your Health During Long-Term Prednisone Therapy
- Blood Pressure and Blood Sugar
- Bone Health
- Weight Management
- Other Considerations
- Medication Interactions
- Tapering Off Prednisone: A Safe and Effective Strategy
- Alternative Treatments to Consider When Weaning Off Prednisone
- Managing Inflammation
- Addressing Underlying Conditions
- Lifestyle Modifications
- Additional Therapies
- Finding Support and Resources for Long-Term Prednisone Management
- Finding Reliable Information
- Practical Tools and Resources
- Additional Support Networks
- Patient Advocacy Groups
Prednisone Long Term: A Detailed Guide
Consult your doctor regularly. This is paramount for managing long-term prednisone use.
Managing Side Effects
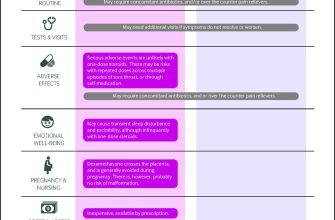
Long-term prednisone use increases your risk of osteoporosis. Daily weight-bearing exercise and a calcium-rich diet are crucial. Your doctor might recommend bone density scans and supplements. Watch for signs of increased blood sugar, like increased thirst or frequent urination. Regular blood glucose monitoring might be necessary. Prednisone can also elevate blood pressure; regular monitoring and lifestyle changes, such as dietary adjustments and exercise, are helpful. Potential weight gain should be addressed through dietary adjustments and exercise, in consultation with your physician.
Tapering Off Prednisone
Never stop prednisone abruptly. Sudden cessation can trigger severe withdrawal symptoms. Your doctor will create a gradual tapering schedule, slowly reducing your dose over weeks or months. This individualized plan minimizes withdrawal effects like fatigue, joint pain, and muscle weakness. Be patient and follow your doctor’s instructions precisely. This method ensures a safer transition off the medication.
Alternative Treatments
Explore alternative therapies alongside prednisone, if your doctor approves. These could include non-steroidal anti-inflammatory drugs (NSAIDs) or biologic medications for your underlying condition. These options can lessen your dependence on prednisone and help minimize side effects over time. Always discuss any alternative treatment options with your doctor to ensure safety and effectiveness.
Monitoring Your Health
Regular checkups are vital. These allow your doctor to monitor your progress, adjust your medication as needed, and promptly address any emerging health concerns. Maintain open communication with your healthcare team to ensure optimal management of your condition and medication.
Lifestyle Adjustments
A healthy lifestyle supports your overall well-being while on long-term prednisone. Maintain a balanced diet, engage in regular exercise, and prioritize sufficient sleep. These habits help mitigate some prednisone side effects and improve your overall health.
Long-Term Prednisone and Mental Health
Prednisone can affect mood. Report any unusual mood changes, such as irritability, anxiety, or depression, to your doctor immediately. Professional mental health support might be beneficial in these cases.
Understanding the Risks of Long-Term Prednisone Use
Prednisone offers significant relief, but prolonged use carries substantial risks. Your doctor should carefully weigh these against the benefits of treatment. Let’s examine the key concerns.
| Risk | Details | Mitigation Strategies |
|---|---|---|
| Osteoporosis | Prednisone weakens bones, increasing fracture risk. This effect is dose-dependent and more pronounced with higher doses and longer durations. | Regular weight-bearing exercise, calcium and vitamin D supplementation, and potential bisphosphonate medication. Regular bone density monitoring is vital. |
| Increased Blood Sugar | Prednisone can raise blood glucose levels, increasing the risk of diabetes or worsening existing diabetes. | Regular blood sugar monitoring, dietary adjustments, and potentially medication to manage blood sugar are needed. Close monitoring by your doctor is critical. |
| Weight Gain | Fluid retention and changes in fat distribution are common side effects, leading to weight gain. | Healthy diet and regular exercise are paramount. Consult a nutritionist for personalized guidance. |
| High Blood Pressure | Prednisone can elevate blood pressure, increasing cardiovascular risk. | Regular blood pressure monitoring and potential medication to control blood pressure are crucial. Lifestyle changes including dietary modifications and stress reduction are beneficial. |
| Cataracts and Glaucoma | Long-term use increases the likelihood of developing cataracts and glaucoma. | Regular eye exams are recommended to detect these conditions early. |
| Increased Infection Risk | Prednisone suppresses the immune system, making you more vulnerable to infections. | Practicing good hygiene, avoiding crowds during flu season, and getting recommended vaccinations are key. Report any signs of infection immediately to your doctor. |
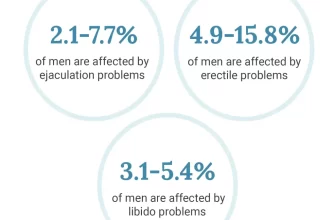
| Mood Changes | Prednisone can cause mood swings, anxiety, and depression. | Open communication with your doctor is crucial. Consider counseling or medication if needed. |
| Muscle Weakness | Prednisone can lead to muscle wasting and weakness. | Regular physical therapy and strength training can help mitigate this. |
This information is for educational purposes only and does not constitute medical advice. Always discuss your treatment plan with your doctor to address your specific needs and concerns. Regular monitoring and open communication are essential for safe and effective long-term prednisone management.
Managing Prednisone Side Effects: A Practical Approach
Consult your doctor regularly to monitor your progress and adjust your dosage as needed. This proactive approach helps minimize long-term complications.
Maintain a healthy diet rich in fruits, vegetables, and lean protein. This supports your body’s ability to cope with the medication’s effects.
Engage in regular, moderate exercise. Aim for at least 30 minutes most days of the week. Walking, swimming, or cycling are excellent options; choose activities you enjoy.
Prioritize adequate sleep. Aim for 7-9 hours of quality sleep each night to promote healing and reduce stress.
Manage your weight. Prednisone can contribute to weight gain; mindful eating and regular exercise counter this effect.
Stay hydrated by drinking plenty of water throughout the day. This helps with many side effects, including constipation.
If you experience insomnia, try relaxation techniques like meditation or deep breathing exercises before bed. Avoid caffeine and alcohol before sleep.
Monitor your blood sugar levels regularly, especially if you have diabetes or a family history. Prednisone can impact blood sugar.
Report any concerning side effects to your doctor immediately. This includes muscle weakness, vision changes, or significant mood swings.
Consider bone density testing to monitor for osteoporosis risk. Prednisone can weaken bones; early detection allows for preventative measures.
Explore support groups or online communities. Connecting with others facing similar challenges provides valuable emotional support and practical advice.
Monitoring Your Health During Long-Term Prednisone Therapy
Schedule regular check-ups with your doctor. These appointments allow for proactive monitoring of blood pressure, blood sugar, bone density, and weight. Frequency depends on your individual needs and health status, but expect at least quarterly visits.
Blood Pressure and Blood Sugar
Monitor your blood pressure and blood sugar regularly at home, as instructed by your physician. Keep a detailed log of these readings to share at your appointments. High blood pressure and elevated blood sugar are common side effects of long-term prednisone use and require careful management. Consider using a blood pressure monitor and glucometer for consistent tracking.
Bone Health
Prednisone can weaken bones, increasing fracture risk. Discuss bone density testing with your doctor. Calcium and Vitamin D supplements may be recommended. Engage in weight-bearing exercises, like walking or weight training, to support bone health.
Weight Management
Prednisone can cause weight gain. Maintain a healthy diet and exercise regularly to mitigate this. Consult a registered dietitian for personalized guidance on nutrition and weight management while on prednisone. Regular weigh-ins are advised.
Other Considerations
Report any new or worsening symptoms to your doctor immediately. These may include muscle weakness, easy bruising, mood changes, cataracts, glaucoma, and increased susceptibility to infections. Your doctor may need to adjust your medication or recommend additional treatments.
Medication Interactions
Inform your doctor and pharmacist about all medications, including over-the-counter drugs and supplements, you are taking. Prednisone can interact with other medications. This step is paramount for avoiding potentially harmful drug interactions.
Always follow your doctor’s instructions regarding medication dosage and scheduling. Never stop taking prednisone abruptly without consulting your physician.
Tapering Off Prednisone: A Safe and Effective Strategy
Always work closely with your doctor to create a personalized tapering schedule. Sudden cessation can be dangerous.
A common approach involves reducing your daily dose by a small amount, usually 5-10mg, every few days or weeks. Your physician will adjust this based on your individual needs and response. For example, you might start by decreasing your dose by 5mg every 3 days, then adjust the frequency and amount as you progress.
Monitor your body closely for signs of withdrawal, such as fatigue, muscle weakness, joint pain, or nausea. Report any concerning symptoms to your doctor immediately. They may adjust your tapering plan to minimize discomfort.
Consider incorporating healthy lifestyle choices to support your body during the tapering process. A balanced diet, regular exercise (as tolerated), and sufficient rest can aid in managing potential side effects.
The length of the tapering period varies depending on several factors, including the initial prednisone dose, duration of treatment, and your overall health. It can take several weeks or even months to safely discontinue prednisone completely.
Your doctor might recommend specific blood tests to monitor your adrenal gland function during the tapering process. This helps ensure your body is adapting adequately to the reduced prednisone levels. Follow their instructions diligently.
Maintaining open communication with your healthcare provider is paramount. Regular check-ups allow for adjustments to the tapering schedule as needed, ensuring a safe and successful transition off prednisone.
Alternative Treatments to Consider When Weaning Off Prednisone
Consult your doctor to explore alternative treatments tailored to your specific condition and needs. They can guide you through a safe and effective weaning process.
Managing Inflammation
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Ibuprofen or naproxen can help reduce inflammation, but use them cautiously due to potential side effects. Always follow your doctor’s instructions regarding dosage and duration.
- Disease-modifying antirheumatic drugs (DMARDs): For autoimmune conditions, DMARDs like methotrexate or sulfasalazine may be prescribed to slow disease progression and reduce inflammation. These medications typically take several weeks to show their full effect.
- Biologics: In some cases, biologics such as TNF inhibitors (e.g., infliximab, adalimumab) may be used to target specific components of the immune system causing inflammation. These are powerful medications with potential side effects, requiring careful monitoring.
Addressing Underlying Conditions
The necessity of alternative treatments often depends on the underlying condition for which prednisone was prescribed. For example, if you were on prednisone for asthma, your doctor might recommend increased use of inhaled corticosteroids or other asthma controllers.
Lifestyle Modifications
- Dietary changes: A balanced diet rich in anti-inflammatory foods (fruits, vegetables, fish) can support your body’s healing process. Discuss any dietary restrictions or needs with your doctor or a registered dietitian.
- Regular exercise: Gentle exercise, such as walking or swimming, can help manage inflammation and improve overall health, but always start slowly and consult your doctor before beginning a new exercise routine.
- Stress reduction techniques: Stress can exacerbate inflammation. Explore stress-reducing practices like yoga, meditation, or deep breathing exercises.
Additional Therapies
- Physical therapy: This can be beneficial for managing pain and improving mobility associated with certain conditions.
- Occupational therapy: For conditions affecting daily tasks, occupational therapy can teach adaptive strategies.
Remember, gradually tapering off prednisone is crucial to avoid adrenal insufficiency. Work closely with your doctor to develop a personalized weaning plan to minimize withdrawal symptoms and ensure a smooth transition to alternative therapies.
Finding Support and Resources for Long-Term Prednisone Management
Connect with others facing similar challenges. Online support groups, like those found on dedicated health forums or social media platforms, offer invaluable peer-to-peer support and shared experiences. These groups provide a safe space to ask questions, share tips, and find emotional encouragement.
Finding Reliable Information
Prioritize credible sources. The National Institutes of Health (NIH) website, reputable medical journals (like the New England Journal of Medicine or the Lancet), and your doctor are excellent starting points for accurate, evidence-based information. Be wary of unverified online information.
- Check the author’s credentials. Is the information backed by scientific studies?
- Look for multiple sources corroborating the information.
- Avoid websites selling products or services alongside health advice.
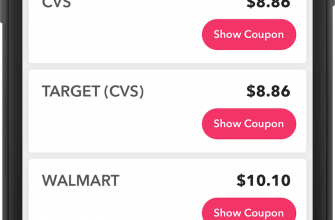
Practical Tools and Resources
- Medication management apps: Many apps help track medication schedules, dosage, and potential side effects.
- Symptom trackers: Record your symptoms to help you and your doctor monitor the effectiveness of your treatment and identify any emerging issues.
- Health diaries: Maintain a diary to note your daily activities, food intake, and any changes in your physical and mental well-being. This aids in identifying potential triggers for side effects.
- Support from healthcare professionals: Regularly schedule appointments with your physician, endocrinologist, and/or other specialists as recommended. Don’t hesitate to discuss concerns. Consider a registered dietitian for dietary advice.
Additional Support Networks
Consider seeking support from mental health professionals. Long-term prednisone use can impact mental health. Therapists and counselors can provide tools to cope with stress, anxiety, or depression. A strong support system of friends and family is also vital. Open communication about your experience is crucial. Don’t isolate yourself.
Patient Advocacy Groups
Investigate patient advocacy groups focused on your specific condition. These organizations often offer valuable resources, including educational materials, workshops, and connections to other individuals facing similar situations.