Prednisone weakens your immune system. This means your body becomes less effective at fighting off infections. Understanding the degree of immunosuppression is key to managing your treatment safely.
The extent of immune suppression depends on the Prednisone dosage and duration of use. High doses, especially over extended periods, carry a significantly higher risk of infections. Common infections, like colds or the flu, can become more severe and prolonged. Opportunistic infections, caused by microbes normally kept in check by a healthy immune system, also pose a greater threat.
Protect yourself: Practice meticulous hygiene – frequent handwashing is critical. Avoid close contact with sick individuals. Consult your doctor immediately if you experience any signs of infection, such as fever, cough, or unusual fatigue. They can adjust your treatment plan or prescribe prophylactic antibiotics if necessary. Regular checkups are also highly recommended during Prednisone therapy. Open communication with your healthcare provider ensures you receive the best possible care and minimizes risks.
Remember: While Prednisone is a powerful medication with numerous benefits, understanding its impact on your immune system allows you to take proactive steps to maintain your health.
- Prednisone’s Impact on Your Immune System
- How Prednisone Suppresses Immune Response
- Increased Risk of Infection While on Prednisone
- Understanding the Risk
- Protecting Yourself
- Specific Infections to Watch For
- Managing Infection Risk During Prednisone Treatment
- Avoiding Illness
- Monitoring Your Health
- Dietary Considerations
- Prednisone and Vaccine Effectiveness
- Tapering Off Prednisone: Restoring Immune Function
Prednisone’s Impact on Your Immune System
Prednisone, a powerful corticosteroid, suppresses your immune system. This means your body’s ability to fight off infections and illnesses reduces significantly.
The extent of immune suppression depends on the dose and duration of Prednisone treatment. Higher doses and longer treatment periods generally lead to greater immune compromise.
- Increased susceptibility to infections: Expect a higher risk of catching common colds, flu, and other infections. Your body’s natural defenses are weakened.
- Slower wound healing: Prednisone interferes with the body’s repair processes, resulting in slower healing of cuts, bruises, and surgical incisions.
- Higher risk of serious infections: In some cases, suppression can lead to more serious, opportunistic infections caused by bacteria, viruses, or fungi normally kept in check by a healthy immune system.
- Reactivation of latent infections: Prednisone can reactivate dormant infections like herpes or tuberculosis.
To minimize risks:
- Practice meticulous hygiene: Frequent handwashing and avoiding close contact with sick individuals are crucial.
- Stay up-to-date on vaccinations: Discuss vaccination strategies with your doctor, as some vaccines might be less effective or contraindicated while on Prednisone.
- Report any signs of infection promptly: Fever, cough, skin rashes, or any unusual symptoms should be reported to your physician immediately.
- Follow your doctor’s instructions carefully: Adhere strictly to the prescribed dose and duration of Prednisone. Never stop taking it without consulting your doctor.
- Maintain a healthy lifestyle: A balanced diet, regular exercise, and sufficient sleep support a stronger immune response, even while on Prednisone.
Open communication with your doctor is key. Discuss any concerns you have about the impact of Prednisone on your immune system.
How Prednisone Suppresses Immune Response
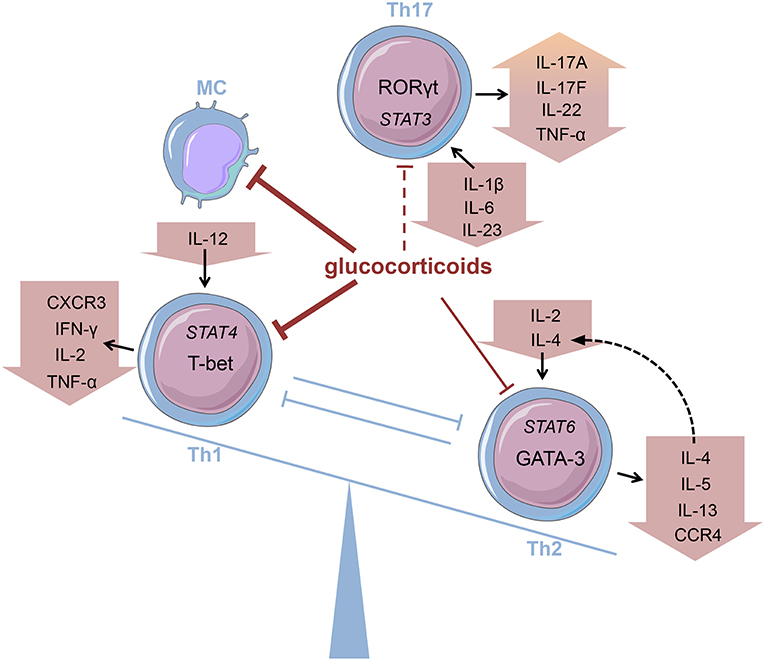
Prednisone, a corticosteroid, directly impacts immune cells, reducing their activity. It achieves this primarily by interfering with the production and release of inflammatory molecules like cytokines. These molecules are crucial signals that coordinate the immune response, activating immune cells to fight infection and inflammation.
Specifically, Prednisone inhibits the transcription of genes responsible for producing these cytokines. This means fewer cytokine signals are sent, leading to a dampened immune response. The drug also reduces the number of circulating white blood cells, particularly lymphocytes, which are key players in adaptive immunity – the body’s targeted response to specific pathogens.
Furthermore, Prednisone affects the function of immune cells themselves. It weakens the ability of these cells to migrate to sites of infection or inflammation, hindering their effectiveness in eliminating threats. This multifaceted action accounts for Prednisone’s immunosuppressive effects.
In short: Prednisone lowers immune function by limiting cytokine production, reducing white blood cell numbers, and impairing immune cell activity.
Note: This information is for educational purposes only and should not replace advice from a healthcare professional. Always consult your doctor regarding Prednisone use and potential side effects.
Increased Risk of Infection While on Prednisone
Prednisone weakens your immune system, making you more vulnerable to infections. This increased susceptibility affects various infections, from common colds to more serious illnesses like pneumonia.
Understanding the Risk
Prednisone’s immunosuppressive effects reduce your body’s ability to fight off bacteria, viruses, and fungi. The higher your Prednisone dosage and the longer you take it, the greater your risk becomes. This risk is especially pronounced for opportunistic infections–infections that typically don’t affect people with healthy immune systems.
Protecting Yourself
Practice diligent hygiene: Frequent handwashing with soap and water remains your best defense. Avoid close contact with individuals exhibiting signs of illness. Maintain good respiratory hygiene by covering your mouth and nose when coughing or sneezing.
Get recommended vaccinations: Discuss with your doctor the need for influenza and pneumococcal vaccines. These offer crucial protection against common infections. Your physician will determine appropriate vaccination schedules based on your individual health status.
Report any symptoms immediately: Even seemingly minor symptoms like fever, cough, or skin rash warrant immediate medical attention. Prompt treatment significantly improves outcomes. Don’t delay seeking care, even if you initially dismiss the symptoms as minor.
Specific Infections to Watch For
Common infections such as colds and the flu can become significantly more serious. Opportunistic infections like shingles (herpes zoster), fungal infections (candidiasis), and tuberculosis pose a heightened risk. Your physician can provide more detailed information about specific infections relevant to your health history and current medications.
Stay informed: Maintain open communication with your healthcare provider about your medication and any health concerns. Regular check-ups aid in early detection and treatment of potential infections.
Managing Infection Risk During Prednisone Treatment
Wash your hands frequently with soap and water for at least 20 seconds, especially before eating and after using the restroom. This simple act significantly reduces your exposure to germs.
Avoiding Illness
Avoid contact with individuals who are sick. Influenza and pneumonia vaccines are highly recommended. Consider wearing a mask in crowded places during cold and flu season. Practice good hygiene – cover coughs and sneezes, and dispose of tissues properly.
Monitoring Your Health
Report any signs of infection to your doctor immediately. These may include fever, chills, cough, sore throat, or any unusual redness or swelling. Prompt attention is key to managing infections effectively. Regular checkups with your doctor allow for proactive monitoring and early detection of potential problems.
Dietary Considerations
Maintain a balanced, nutritious diet rich in fruits and vegetables to support your immune system. Sufficient hydration is also critical. Your doctor can provide personalized recommendations based on your specific needs and any existing health conditions.
Prednisone and Vaccine Effectiveness
Consult your doctor before receiving any vaccine while taking prednisone. Prednisone suppresses your immune system, potentially reducing the effectiveness of vaccines.
The extent of this reduction depends on several factors: the prednisone dosage, the duration of treatment, and the type of vaccine. Higher doses and longer treatment periods generally lead to greater immune suppression.
Live vaccines, such as the measles, mumps, rubella (MMR) vaccine and the varicella (chickenpox) vaccine, pose a higher risk of complications when taken while on prednisone due to their use of a weakened, but still live, virus. These vaccines should generally be avoided during prednisone treatment unless your doctor determines the benefit outweighs the risk.
Inactivated vaccines, which use killed viruses or parts of viruses, may still be less effective when taken during prednisone use. Your doctor may recommend delaying vaccination until after you complete your prednisone course.
Antibody responses to vaccines may be lower while on prednisone. This means your body might not produce enough antibodies to protect you from the disease the vaccine targets. Your doctor can monitor your antibody levels after vaccination to assess the response.
Always discuss your medication regimen with your doctor before scheduling any vaccinations. They will assess your individual situation to determine the safest and most appropriate course of action.
Tapering Off Prednisone: Restoring Immune Function
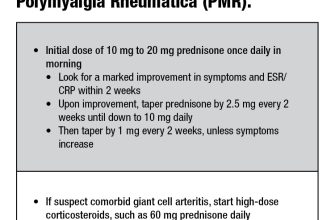
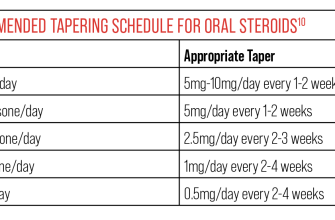
Gradually reduce your Prednisone dosage as directed by your doctor. This prevents sudden immune system shock.
Maintain a healthy diet rich in fruits, vegetables, and whole grains. These provide essential vitamins and antioxidants supporting immune cell production.
Prioritize sleep. Aim for 7-9 hours of quality sleep nightly. Sleep deprivation weakens your immune response.
Engage in regular moderate exercise. Physical activity boosts circulation and improves immune cell function. Consult your doctor before starting any new exercise routine.
Manage stress levels. Chronic stress suppresses the immune system. Explore stress-reduction techniques like yoga, meditation, or deep breathing exercises.
Avoid close contact with sick individuals. Your immune system will be recovering, so reduce exposure to infections.
Stay hydrated. Adequate fluid intake supports bodily functions, including immune responses.
Consider probiotic supplements. These can help restore gut flora, crucial for a healthy immune system. Discuss this with your doctor.
Monitor for signs of infection, such as fever, cough, or fatigue. Report any concerning symptoms to your physician immediately.
Schedule regular check-ups with your doctor to monitor your immune system’s recovery and adjust your tapering schedule accordingly.