Prednisone significantly reduces your body’s inflammatory response. This means it lowers the activity of your immune system, making you more susceptible to infections.
This immunosuppressive effect is dose-dependent; higher doses lead to greater suppression. For instance, a low dose might slightly weaken your immune response, while a high dose could leave you vulnerable to serious infections.
Consequently, monitor for any signs of infection, such as fever, cough, or unusual fatigue. Report these symptoms to your doctor immediately. Regular blood tests can also help track your immune function while taking prednisone.
Remember, the duration of prednisone use directly impacts immune suppression. Prolonged use generally increases your risk of infections. Discuss tapering strategies with your physician to minimize long-term immune compromise. This gradual reduction allows your immune system to recover more effectively.
Always consult your doctor before starting or stopping prednisone. They can help manage potential risks and ensure you receive appropriate monitoring.
- Prednisone and Immune Suppression: A Detailed Overview
- Understanding the Mechanism
- Increased Infection Risk
- Minimizing Risks
- Conclusion
- How Prednisone Works to Suppress the Immune System
- Common Side Effects Related to Immune Suppression from Prednisone
- Increased Infection Risk: Specific Considerations
- Other Potential Side Effects
- Increased Risk of Infections While on Prednisone
- Managing Infections While Taking Prednisone
- Recognizing Infection Symptoms
- Medication Adherence
- Vaccination
- Prednisone and Vaccination: Important Considerations
- Tapering Off Prednisone to Minimize Immune System Impact
- Long-Term Effects of Prednisone on the Immune System
Prednisone and Immune Suppression: A Detailed Overview
Prednisone, a corticosteroid, significantly weakens your immune system. This means your body becomes less capable of fighting off infections and diseases.
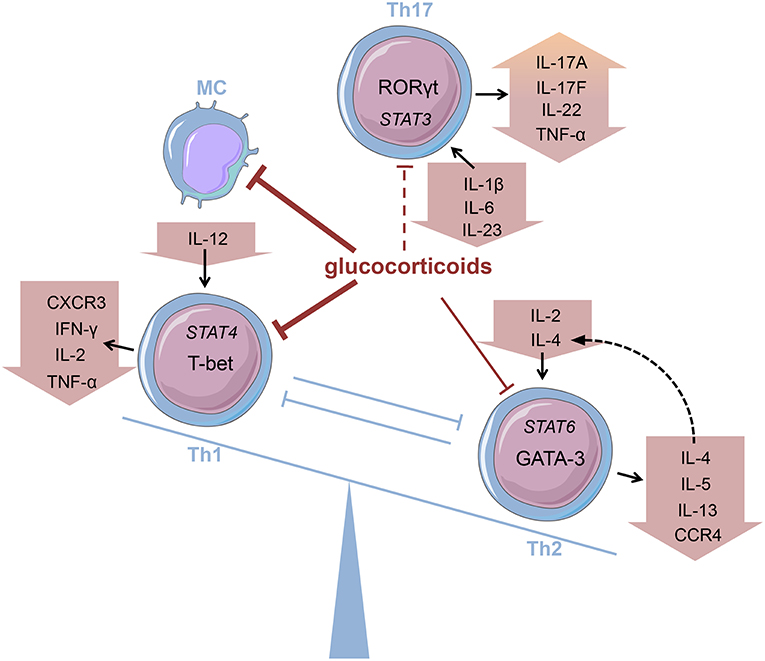
Understanding the Mechanism
Prednisone works by reducing the activity of your immune cells, including lymphocytes (T cells and B cells) and macrophages. This decrease in immune cell function lowers inflammation, which is helpful for managing conditions like asthma and rheumatoid arthritis. However, this also leaves you more vulnerable to infections.
- Reduced Lymphocyte Production: Prednisone hampers the production of new lymphocytes, reducing your body’s ability to mount an effective immune response.
- Impaired Phagocytosis: Macrophages, crucial for engulfing and destroying pathogens, become less effective under the influence of prednisone.
- Antibody Suppression: Antibody production, vital for targeted immune defense, also decreases with prednisone use.
Increased Infection Risk
The weakened immune response translates to a higher risk of infections. These can range from mild, like the common cold, to severe, such as pneumonia or tuberculosis. You’re more susceptible to opportunistic infections – infections caused by microorganisms that typically wouldn’t cause illness in a person with a healthy immune system.
- Viral Infections: Prednisone increases the likelihood of contracting viral infections, including herpes zoster (shingles).
- Bacterial Infections: Bacterial infections, like pneumonia and urinary tract infections, become more common and severe.
- Fungal Infections: Prednisone can exacerbate existing fungal infections and increase susceptibility to new ones.
Minimizing Risks
Several strategies can help mitigate the immune-suppressing effects of prednisone:
- Vaccination: Discuss with your doctor about appropriate vaccinations. Some vaccines might be less effective while on prednisone.
- Hygiene Practices: Maintaining rigorous hygiene, including frequent handwashing, can reduce exposure to pathogens.
- Infection Monitoring: Promptly report any signs of infection to your doctor, even if seemingly minor. Early intervention is key.
- Dosage Management: Your doctor carefully monitors your prednisone dosage to find the lowest effective dose and minimize immune suppression.
- Lifestyle Changes: A healthy lifestyle, including proper nutrition and adequate sleep, supports immune function.
Conclusion
Prednisone’s impact on the immune system necessitates careful monitoring and proactive measures. By understanding the risks and implementing preventive strategies, individuals can use prednisone effectively while minimizing potential complications.
How Prednisone Works to Suppress the Immune System
Prednisone, a corticosteroid, mimics the effects of cortisol, a hormone your body naturally produces. This hormone regulates inflammation and immune responses. Prednisone achieves immune suppression by binding to specific receptors inside immune cells, like lymphocytes (T cells and B cells) and macrophages.
This binding alters gene expression within these cells, reducing the production of inflammatory molecules like cytokines. Fewer cytokines mean less signaling between immune cells, dampening their activity. Specifically, it inhibits the production of interleukin-1, interleukin-6, and tumor necrosis factor-alpha, key players in inflammation and immune responses.
Prednisone also affects the immune system by reducing the number of circulating white blood cells, including those involved in cell-mediated immunity. This decrease in cell count limits the body’s ability to mount an effective immune response to foreign invaders.
Finally, prednisone impedes the movement of immune cells to sites of inflammation. This limits their ability to attack perceived threats, further reducing inflammation and immune response intensity. The overall effect is a significant reduction in the body’s immune activity.
Common Side Effects Related to Immune Suppression from Prednisone
Prednisone’s immune suppression increases your susceptibility to infections. Expect a heightened risk of common colds, flu, and more serious infections like pneumonia or herpes zoster (shingles). Practice diligent hygiene: wash your hands frequently and avoid close contact with sick individuals. Consult your doctor immediately if you experience fever, persistent cough, or unusual fatigue.
Increased Infection Risk: Specific Considerations
Certain infections may appear more frequently or severely in people taking Prednisone. For example, fungal infections (like oral thrush or yeast infections) are more common. Bacterial infections, including those of the skin and urinary tract, might also be more problematic. Your doctor might suggest preventative measures based on your individual risk profile. Report any new or worsening skin lesions, changes in urination, or other signs of infection without delay.
Weakened immunity also makes you vulnerable to opportunistic infections – those caused by microorganisms that usually don’t cause disease in people with healthy immune systems. Early detection is key; regular check-ups with your physician are recommended while you’re on Prednisone.
Other Potential Side Effects
Beyond infections, immune suppression from Prednisone can manifest in other ways. You might notice increased bruising or slow wound healing, because your body’s ability to repair tissues is impacted. Monitor your skin carefully and avoid activities that could increase the risk of injury. If you notice prolonged bleeding or unusually easy bruising, contact your doctor immediately.
Increased Risk of Infections While on Prednisone
Prednisone weakens your immune system, making you more vulnerable to infections. This increased susceptibility applies to various infections, from common colds to more serious illnesses like pneumonia.
Monitor yourself closely for any signs of infection, such as fever, cough, sore throat, or unusual fatigue. Report any symptoms to your doctor immediately. Early detection and treatment are key to managing infections effectively.
Practice diligent hygiene. Wash your hands frequently with soap and water, and avoid close contact with individuals who are sick. Regular hand sanitization is also helpful.
Avoid contact with individuals who have contagious illnesses, such as the flu or chickenpox. Consider getting recommended vaccinations, such as the flu shot, to bolster your protection. Your doctor can advise on appropriate vaccinations for your specific situation.
Maintain a healthy lifestyle. Proper nutrition, adequate rest, and stress management help support your immune system. A balanced diet and sufficient sleep are especially important when taking prednisone.
Your doctor might suggest preventive measures based on your individual health status and prednisone dosage. Open communication with your doctor is crucial for managing the risks associated with prednisone.
Managing Infections While Taking Prednisone
Wash your hands frequently with soap and water for at least 20 seconds. This simple act significantly reduces your risk of infection.
Avoid contact with sick individuals. Influenza and other common illnesses pose a greater threat when your immune system is suppressed.
Maintain a balanced diet rich in fruits and vegetables. Proper nutrition supports your body’s natural defenses.
Get enough sleep. Adequate rest is crucial for immune function and overall health.
Recognizing Infection Symptoms
Pay close attention to any changes in your body. Symptoms like fever, cough, sore throat, or unusual fatigue require immediate medical attention.
Don’t delay seeking medical help if you suspect an infection. Early intervention is key to effective treatment.
Medication Adherence
Strictly follow your doctor’s instructions regarding Prednisone dosage and schedule. Improper use can worsen your condition.
Communicate openly with your doctor about any side effects or concerns. They can adjust your treatment plan accordingly.
| Symptom | Possible Infection | Action |
|---|---|---|
| High fever (100.4°F or higher) | Bacterial or viral infection | Contact your doctor immediately |
| Persistent cough | Respiratory infection (e.g., pneumonia) | Seek medical advice |
| Severe sore throat | Strep throat | Visit your doctor for a diagnosis |
| Skin rash or lesions | Skin infection | Consult a dermatologist |
Vaccination
Discuss vaccination options with your doctor. Annual influenza and pneumonia vaccines can offer crucial protection.
Your doctor can determine which vaccines are safe and appropriate for you while on Prednisone.
Prednisone and Vaccination: Important Considerations
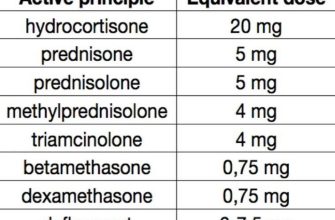
Talk to your doctor before scheduling any vaccinations while taking prednisone. Prednisone weakens your immune system, potentially reducing the effectiveness of vaccines.
The level of immunosuppression depends on the prednisone dose and duration of treatment. High doses for extended periods significantly impair your body’s ability to mount a protective immune response.
Some vaccines, like live attenuated vaccines (e.g., MMR, varicella, and the nasal flu vaccine), carry a higher risk of complications when administered during prednisone use. Your doctor will likely recommend delaying these until your prednisone course is complete and your immune system recovers.
Inactivated vaccines (e.g., flu shot, polio vaccine) pose a lower risk, but their efficacy may still be reduced. Your physician will weigh the benefits and risks based on your specific circumstances.
Timing is key. Discuss your vaccination schedule with your doctor to determine the optimal time for vaccination after you finish your prednisone treatment. This allows your immune system sufficient time to recover before receiving the vaccine.
Monitor for any unusual reactions after vaccination. Report any concerning symptoms, such as fever, rash, or prolonged pain at the injection site, to your healthcare provider immediately.
Remember: Open communication with your doctor is vital for safe and effective vaccination while on prednisone. Your doctor’s expertise will ensure you receive the necessary vaccinations while minimizing potential risks.
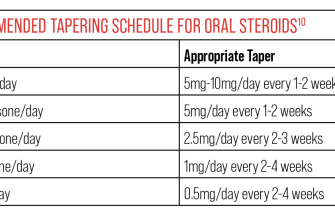
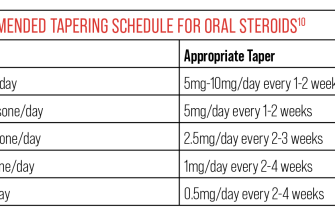
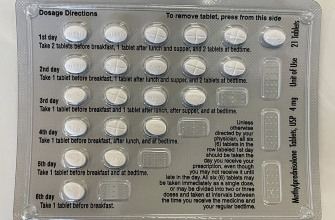
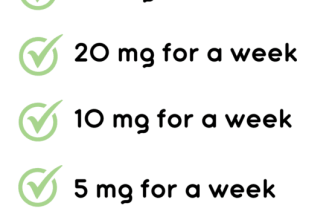
Tapering Off Prednisone to Minimize Immune System Impact
Always follow your doctor’s instructions precisely. Your doctor will create a personalized tapering schedule based on your specific needs and health history. This schedule usually involves gradually decreasing your prednisone dosage over several weeks or months, not abruptly stopping.
Expect potential side effects during tapering. These can include fatigue, joint pain, and increased susceptibility to infections. Monitor yourself closely and report any concerns to your doctor immediately.
Maintain a healthy lifestyle. Prioritize sufficient sleep, a balanced diet rich in fruits and vegetables, and regular, moderate exercise to support your immune system recovery. These habits can help mitigate the negative effects of prednisone withdrawal.
Consider supplements. Discuss with your doctor the possibility of taking supplements like vitamin D and probiotics, which can support immune function. They might recommend additional supplements depending on your individual needs.
Be patient and consistent. The process of tapering off prednisone takes time. Strict adherence to your doctor’s plan is crucial for minimizing the impact on your immune system and preventing potential complications. Regular check-ups with your physician are necessary to monitor your progress and adjust your treatment plan as needed.
Report any infections promptly. Because your immune system is suppressed, even minor infections can become more serious. Seek medical attention immediately if you develop any symptoms of infection, such as fever, cough, or sore throat.
Long-Term Effects of Prednisone on the Immune System
Prolonged Prednisone use significantly weakens your immune system, increasing susceptibility to infections. This effect is dose-dependent and duration-dependent; higher doses and longer treatment periods lead to greater immunosuppression.
Here’s what you should know:
- Increased Infection Risk: Expect a higher chance of catching common illnesses like colds, flu, and more serious infections. Bacterial, viral, and fungal infections become more likely.
- Slowed Wound Healing: Prednisone interferes with the body’s natural healing processes, potentially delaying the recovery of cuts, scrapes, and surgical wounds.
- Reactivation of Latent Infections: Conditions like herpes simplex, tuberculosis, and chickenpox can be reactivated due to weakened immunity.
- Impaired Vaccine Response: Your body’s ability to respond to vaccines may be reduced, decreasing the effectiveness of immunizations.
- Increased Risk of Opportunistic Infections: Prednisone can make you vulnerable to infections caused by organisms that usually don’t cause disease in healthy individuals.
To mitigate these risks:
- Maintain close communication with your doctor: Regular check-ups are crucial to monitor your health and adjust your Prednisone dosage as needed.
- Practice diligent hygiene: Frequent handwashing and avoiding contact with sick individuals can significantly reduce your infection risk.
- Get recommended vaccinations: Discuss vaccination schedules with your physician; some may be less effective or contraindicated during Prednisone treatment.
- Report any signs of infection promptly: Fever, cough, skin rashes, or any unusual symptoms should be reported immediately to your doctor.
- Consider preventative measures: Your doctor might suggest antiviral or antifungal medications to reduce the risk of specific infections, based on your individual risk profile.
Remember, tapering off Prednisone should always be done under medical supervision to minimize the impact on your immune system. Never stop taking Prednisone abruptly.