Prednisone can cause fluid retention, leading to swelling in your hands, feet, and face. This is a common side effect, and understanding how to manage it is key to feeling better. Drink plenty of water – counterintuitive, but it helps flush out excess fluid.
Dietary changes matter too. Reduce your sodium intake significantly. Processed foods are major culprits; opt for fresh fruits, vegetables, and lean proteins. Consider limiting alcohol and caffeine, which can exacerbate fluid retention. Regular exercise helps, even a moderate daily walk improves circulation and can help with fluid management.
Consult your doctor. They can monitor your condition and adjust your prednisone dosage or prescribe diuretics if necessary. Don’t self-treat. Open communication with your doctor is crucial for managing this side effect safely and effectively. They might also suggest other strategies tailored to your individual needs and health status.
Remember: While water retention is common, it’s not inevitable. Proactive management with these strategies can significantly minimize its impact on your well-being.
- Prednisone Water Retention: A Detailed Guide
- Understanding Prednisone’s Effect on Fluid Balance
- Recognizing the Signs and Symptoms of Prednisone-Induced Water Retention
- Swelling: Where to Look
- Other Symptoms to Watch For
- When to Seek Medical Attention
- Factors Influencing Water Retention Severity While on Prednisone
- Dietary and Lifestyle Adjustments to Minimize Water Retention
- Medical Management Strategies for Prednisone-Related Edema
- When to Seek Medical Attention for Water Retention on Prednisone
- Other Warning Signs Requiring Immediate Medical Attention
Prednisone Water Retention: A Detailed Guide
Reduce sodium intake. Lowering your salt consumption significantly helps manage fluid retention. Aim for less than 2,300 milligrams daily.
Increase potassium intake. Potassium helps balance sodium levels, counteracting fluid retention. Good sources include bananas, sweet potatoes, and spinach. Consult your doctor before significantly altering your potassium intake.
Drink plenty of water. Counterintuitive, but adequate hydration helps your kidneys flush out excess fluids more efficiently.
Elevate your legs. This simple act can improve circulation and reduce swelling in your lower extremities.
Wear compression stockings. These garments provide gentle pressure, aiding circulation and minimizing swelling.
Regular exercise. Physical activity boosts circulation and promotes fluid removal. Start slowly and gradually increase intensity as tolerated.
Monitor your weight. Regular weigh-ins help you track fluid retention and adjust your management strategies accordingly.
Consult your physician. This guide provides suggestions, but individualized advice from your doctor is paramount. They can assess your specific needs and adjust your prednisone dosage or prescribe diuretics if necessary. They can also rule out other causes for fluid retention.
Note: This information is for general knowledge and shouldn’t replace professional medical advice. Always consult your doctor before making any changes to your medication or treatment plan.
Understanding Prednisone’s Effect on Fluid Balance
Prednisone, a corticosteroid, increases your body’s sodium retention. This means your kidneys hold onto more sodium, and since water follows sodium, you retain more water.
This fluid retention primarily manifests as swelling (edema), often noticeable in the face, legs, and ankles. The severity varies depending on dosage and individual sensitivity.
- Higher doses generally lead to more significant water retention.
- Longer treatment durations also increase the risk of fluid buildup.
- Pre-existing conditions, such as heart or kidney disease, can exacerbate fluid retention.
Here’s what you can do to manage prednisone-induced water retention:
- Monitor your weight daily: Sudden weight gain often indicates fluid retention. Report significant changes to your doctor.
- Reduce sodium intake: Limit processed foods, fast food, and salty snacks. Choose fresh fruits, vegetables, and lean proteins.
- Increase potassium intake: Potassium helps balance sodium levels. Good sources include bananas, potatoes, and spinach. Always discuss potassium supplements with your doctor.
- Stay hydrated: Drink plenty of water to help flush out excess sodium. However, avoid excessive fluid intake, especially before bed.
- Elevate your legs: This can help reduce swelling in your lower extremities.
- Regular exercise: Helps improve circulation and reduce fluid retention.
- Talk to your doctor: They can adjust your medication or suggest additional strategies to manage fluid retention. They may also prescribe diuretics.
Remember, managing water retention involves a multi-faceted approach. Consulting your healthcare provider is crucial for personalized advice and monitoring.
Recognizing the Signs and Symptoms of Prednisone-Induced Water Retention
Pay close attention to changes in your body. Weight gain, often appearing suddenly, is a primary indicator. This isn’t necessarily fat; it’s fluid retention. A scale can be helpful, but don’t rely solely on it.
Swelling: Where to Look
Notice swelling? Check your ankles, feet, and lower legs first. Facial puffiness and swelling in your hands are also common. Gentle pressure leaving an indentation (pitting edema) points to fluid buildup.
Other Symptoms to Watch For
Shortness of breath can result from fluid accumulating in your lungs. High blood pressure is another potential complication. Feeling unusually bloated or tight in your abdomen is also possible. Consult your doctor immediately if you experience any of these symptoms.
When to Seek Medical Attention
Don’t hesitate to contact your physician if you notice significant weight gain (several pounds in a short period), experience severe swelling, or develop shortness of breath. Early intervention is key to managing this side effect.
Factors Influencing Water Retention Severity While on Prednisone
Your individual response to Prednisone, including water retention, depends on several factors. Understanding these can help you manage any related symptoms.
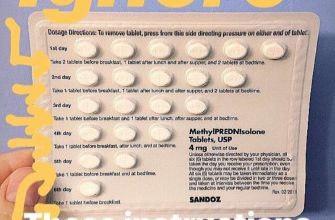
Dosage plays a significant role. Higher doses generally lead to more pronounced fluid retention. Your doctor carefully considers your needs when prescribing the medication; adhering to the prescribed dosage is vital for minimizing side effects.
Duration of treatment is another key factor. Longer courses of Prednisone increase the likelihood of experiencing water retention. Regular check-ups with your doctor help monitor the effects of the medication and adjust the treatment plan as needed.
Pre-existing conditions can significantly influence how your body responds. For example, individuals with heart or kidney problems may experience more severe water retention. Open communication with your doctor about your medical history is critical for effective management.
Diet and hydration also contribute. A high-sodium diet exacerbates fluid retention. Reducing sodium intake and ensuring adequate hydration can mitigate the effect. Your doctor or a registered dietitian can guide you on appropriate dietary adjustments.
Finally, individual genetic factors and your overall health can influence the severity of water retention. Some people are simply more susceptible to Prednisone’s side effects than others. This highlights the importance of personalized medical care.
| Factor | Impact on Water Retention | Actionable Recommendation |
|---|---|---|
| Dosage | Higher doses increase retention. | Follow prescribed dosage meticulously. |
| Treatment Duration | Longer treatment increases risk. | Attend regular check-ups. |
| Pre-existing Conditions | Heart/kidney issues increase severity. | Disclose full medical history to your doctor. |
| Diet | High sodium exacerbates retention. | Reduce sodium intake; consult a dietitian. |
| Genetics & Overall Health | Individual susceptibility varies. | Open communication with your healthcare provider. |
Dietary and Lifestyle Adjustments to Minimize Water Retention
Reduce sodium intake significantly. Aim for less than 2,300 milligrams per day, ideally closer to 1,500mg. Processed foods are major culprits; choose fresh produce, lean proteins, and whole grains instead.
Increase potassium consumption. Potassium helps balance sodium levels. Good sources include bananas, sweet potatoes, spinach, and beans.
Drink plenty of water. Paradoxical as it sounds, dehydration can actually worsen water retention. Aim for at least eight glasses daily.
Limit alcohol consumption. Alcohol is a diuretic initially, but it can ultimately lead to fluid retention.
Moderate your caffeine intake. Caffeine can also have a diuretic effect but may contribute to fluid imbalances if consumed excessively.
Elevate your legs when resting. This promotes better circulation and can reduce fluid pooling in the lower extremities.
Engage in regular, moderate exercise. Physical activity boosts circulation and helps eliminate excess fluid.
Consider a low-carbohydrate diet. High carbohydrate intake can lead to increased insulin levels, potentially promoting water retention. Consult your doctor before making significant dietary changes.
Monitor your weight regularly. Consistent weight gain might indicate worsening water retention, prompting you to adjust your diet or lifestyle.
Medical Management Strategies for Prednisone-Related Edema
Your doctor will tailor treatment to your specific needs and the severity of your edema. Lowering your prednisone dose is often the primary goal. This should be done gradually under close medical supervision to avoid withdrawal symptoms.
Dietary changes can help. Reduce sodium intake significantly; aim for less than 2,000 milligrams per day. Increase potassium-rich foods like bananas and sweet potatoes to counter potassium loss induced by prednisone. Drink plenty of water; adequate hydration aids fluid balance.
If fluid retention is severe, diuretics (water pills) may be prescribed. These medications help your body excrete excess fluid. Common examples include spironolactone (Aldactone) or furosemide (Lasix). Your physician will monitor your potassium levels closely if you’re on a diuretic.
Compression stockings can offer relief from leg swelling by improving circulation. Elevating your legs whenever possible further assists venous return and reduces swelling.
Regular exercise, such as walking, promotes fluid movement and can contribute to overall well-being. However, always consult your physician before starting any new exercise program, especially while on prednisone.
Close monitoring of weight and blood pressure is crucial. Consistent weight gain and elevated blood pressure can indicate worsening edema and require adjustments to your treatment plan. Report any changes immediately to your healthcare provider.
When to Seek Medical Attention for Water Retention on Prednisone
Contact your doctor immediately if you experience sudden, significant weight gain (more than 2 pounds in a day or 5 pounds in a week), especially accompanied by shortness of breath, swelling in your face or legs, or chest pain. These symptoms could indicate serious complications.
Other Warning Signs Requiring Immediate Medical Attention
Seek medical help if water retention is accompanied by: severe headache, visual disturbances (blurred vision, double vision), severe abdominal pain, or changes in your urine output (significantly decreased or increased volume).
While some water retention is common with Prednisone, persistent or worsening swelling warrants a check-up. Don’t hesitate to contact your healthcare provider if you have concerns about your symptoms. Regular monitoring can help prevent serious issues.