Yes, almost always. Prednisone, a powerful corticosteroid, carries significant risks with long-term use. Sudden cessation can trigger serious withdrawal symptoms, so a gradual reduction, or tapering, under medical supervision is vital. This process allows your body to adjust naturally, minimizing potential side effects.
Your doctor will create a personalized tapering schedule based on your individual needs, the dosage you’ve been taking, and your overall health. This plan might involve slowly decreasing your daily dose over several weeks or even months. Factors like your specific condition and response to treatment significantly influence the tapering duration.
Expect regular monitoring during this period. Your physician will track your symptoms and make adjustments to the schedule as needed. Open communication with your doctor is key. Report any concerning symptoms, such as fatigue, muscle weakness, or joint pain, immediately. Early identification and management of withdrawal effects can ensure a smoother transition.
Remember, never stop taking prednisone abruptly without consulting your doctor. Ignoring this crucial step risks severe consequences, including adrenal insufficiency. Prioritize your health and safety by collaborating closely with your healthcare team throughout the entire tapering process.
- Should Prednisone Be Tapered Off?
- Understanding Prednisone Withdrawal
- Tapering Strategies: A Collaborative Approach
- Factors Influencing Tapering Schedules
- Ignoring the Tapering Process: Risks Involved
- Seeking Professional Guidance
- Understanding Prednisone’s Effects on the Body
- Metabolic Effects
- Immunological Effects
- Musculoskeletal Effects
- Other Potential Side Effects
- Important Note:
- The Dangers of Sudden Prednisone Withdrawal
- Creating a Safe Prednisone Tapering Schedule
- Common Symptoms During Prednisone Tapering
- Managing Symptoms During Tapering: Practical Tips
- Communicate with your doctor regularly.
- Listen to your body.
- Maintain a healthy lifestyle.
- Expect some discomfort.
- Monitoring Your Progress and Consulting Your Doctor
- Blood Pressure and Weight Monitoring
- Important Signs to Report to Your Doctor
- Example of a Symptom Tracking Table
- Communicating with Your Doctor
- When to Seek Immediate Medical Attention
Should Prednisone Be Tapered Off?
Yes, prednisone should almost always be tapered off, never stopped abruptly. Sudden cessation can lead to serious withdrawal symptoms.
Understanding Prednisone Withdrawal
Your body adapts to prednisone, suppressing your natural cortisol production. Stopping suddenly leaves your body deficient, causing symptoms like fatigue, muscle weakness, nausea, and even potentially life-threatening adrenal insufficiency.
- Fatigue and weakness: Common symptoms requiring rest and gradual activity increase.
- Nausea and vomiting: May necessitate adjustments to your diet and medication schedule.
- Joint and muscle pain: Consider over-the-counter pain relievers under medical supervision.
- Adrenal insufficiency: A serious condition requiring immediate medical attention.
Tapering Strategies: A Collaborative Approach
Your doctor will design a personalized tapering plan based on your individual needs, the dosage, and duration of prednisone use. This usually involves gradually reducing your dose over weeks or months.
- Regular monitoring: Blood tests may be needed to check cortisol levels and adjust the tapering schedule accordingly.
- Dose reduction schedule: Your doctor will provide a detailed plan outlining the specific reductions in dosage and their timing.
- Symptom management: Your doctor will help manage withdrawal symptoms.
- Open communication: Report any concerning symptoms to your doctor immediately.
Factors Influencing Tapering Schedules
The tapering process varies. Several factors influence the schedule:
- Dosage: Higher doses require longer tapering periods.
- Duration of treatment: Longer treatment periods typically necessitate slower tapering.
- Underlying health conditions: Pre-existing conditions can influence the tapering speed and require close monitoring.
- Individual response: Your body’s response to the medication determines the pace of tapering.
Ignoring the Tapering Process: Risks Involved
Abrupt discontinuation of prednisone poses significant health risks. It’s crucial to follow your doctor’s instructions meticulously. Ignoring the tapering process can lead to severe health complications and prolong recovery time.
Seeking Professional Guidance
Never attempt to adjust your prednisone dosage without consulting your physician. Your doctor is the best resource for creating a safe and effective tapering plan.
Understanding Prednisone’s Effects on the Body
Prednisone, a corticosteroid, powerfully impacts numerous bodily systems. Its effects are dose-dependent, meaning higher doses lead to more pronounced changes.
Metabolic Effects
- Increased Blood Sugar: Prednisone raises blood glucose levels, potentially exacerbating diabetes or causing new-onset diabetes. Regular blood sugar monitoring is crucial.
- Weight Gain: Fluid retention and altered fat distribution contribute to weight gain, often concentrated in the face and abdomen.
- Increased Appetite: Many experience heightened hunger, leading to increased caloric intake and further weight gain. Careful diet management is recommended.
Immunological Effects
Prednisone suppresses the immune system, making you more susceptible to infections. This effect is dose-related; higher doses produce greater immunosuppression.
- Increased risk of infections.
- Delayed wound healing.
- Increased vulnerability to opportunistic infections.
Musculoskeletal Effects
- Muscle Weakness: Prednisone can weaken muscles, leading to fatigue and decreased strength. Regular gentle exercise can help mitigate this.
- Bone Loss (Osteoporosis): Long-term prednisone use increases the risk of osteoporosis. Calcium and Vitamin D supplements, along with weight-bearing exercise, may be necessary.
- Increased risk of fractures.
Other Potential Side Effects
- Mood Changes: Irritability, anxiety, and depression are possible. Mental health support may be beneficial.
- High Blood Pressure: Prednisone can elevate blood pressure, requiring monitoring and potential medication adjustments.
- Fluid Retention (Edema): Swelling in the legs and ankles is a common side effect.
- Thinning Skin: Prednisone can make skin more fragile and prone to bruising.
- Cataracts and Glaucoma: Long-term use increases the risk of these eye conditions.
Important Note:
This information is for educational purposes only and does not constitute medical advice. Always consult your doctor or other qualified healthcare professional for any questions regarding your health or treatment.
The Dangers of Sudden Prednisone Withdrawal
Never stop taking prednisone abruptly. Doing so can trigger serious health problems.
Your body adjusts to prednisone, suppressing its natural cortisol production. Stopping suddenly leaves you with dangerously low cortisol levels. This adrenal insufficiency can manifest as fatigue, muscle weakness, nausea, vomiting, and even life-threatening hypotension.
Symptoms often appear within days of cessation. You may experience severe joint pain, as well as significant mood swings and depression.
Specific risks depend on dosage and duration of treatment. Higher doses and longer treatment periods increase the chance of severe withdrawal symptoms.
Always consult your doctor to create a gradual tapering schedule. This ensures your body adjusts safely, minimizing potential risks.
Your physician will monitor your progress and adjust the tapering schedule as needed, preventing uncomfortable and potentially harmful side effects.
A properly managed withdrawal minimizes the likelihood of adverse reactions, allowing you to transition safely off prednisone.
Ignoring medical advice and stopping prednisone without guidance could lead to serious health consequences. Prioritize your health and follow your doctor’s instructions.
Creating a Safe Prednisone Tapering Schedule
Always work closely with your doctor to design your tapering plan. They’ll consider your specific health situation and prednisone dosage. A gradual reduction is key.
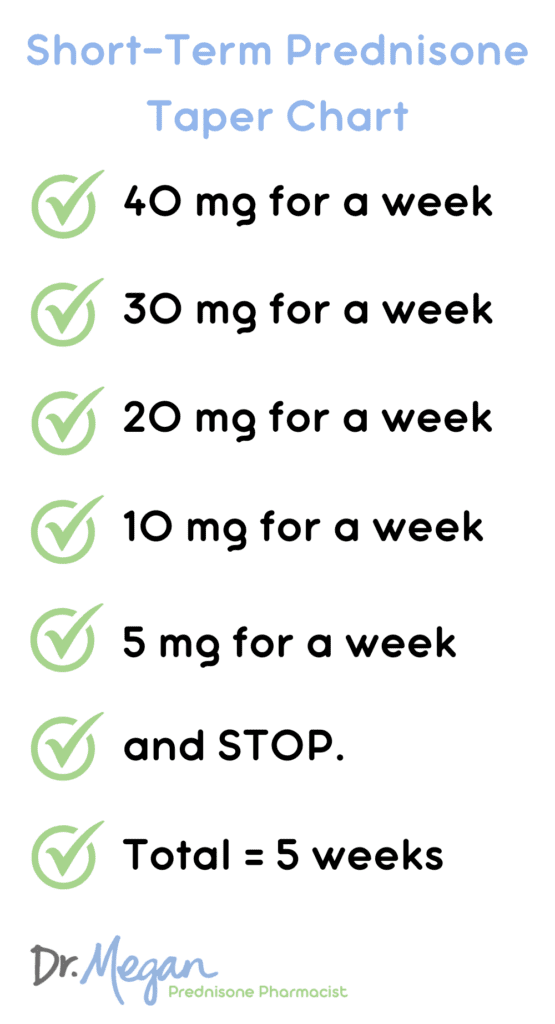
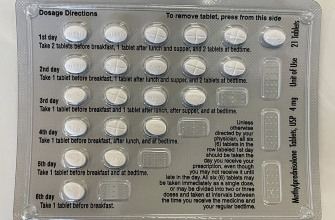
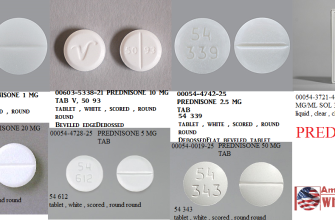
Typical Tapering Schedules: Doctors often recommend decreasing your dose by 5-10mg every few days or weeks, depending on the initial dose and your body’s response. For example, if you’re on 40mg, you might drop to 35mg for a week, then 30mg, and so on. Lower doses might require smaller decrements, perhaps 2.5mg.
Important Note: Never stop prednisone abruptly. Sudden cessation can trigger serious withdrawal symptoms like fatigue, muscle weakness, joint pain, and even adrenal insufficiency.
Monitoring Your Progress: Regular check-ups are vital. Your doctor will monitor your symptoms and adjust the tapering schedule accordingly. Be sure to report any new or worsening symptoms immediately. Blood tests may be used to monitor your adrenal function.
Factors Influencing Tapering: Your individual response to prednisone significantly impacts the tapering process. Pre-existing health conditions, the duration of prednisone use, and your overall health all influence the speed and safety of reduction.
Alternative Approaches: In certain cases, alternate-day dosing might be an option. This involves taking your full dose every other day. Discuss this alternative with your physician; it’s not suitable for all patients.
Managing Withdrawal Symptoms: Some discomfort during tapering is common. Your doctor might suggest strategies to manage symptoms, such as pain relievers or other medications. Maintaining a healthy lifestyle – including adequate rest, nutrition, and hydration – is crucial for supporting your body during this process.
Remember: Your doctor is your best resource for creating a personalized and safe prednisone tapering schedule. Open communication and close monitoring are fundamental for a successful outcome.
Common Symptoms During Prednisone Tapering
Expect fatigue and weakness as your body adjusts. These are common and often improve as you continue tapering. Stay hydrated and prioritize rest.
Joint and muscle pain can appear, sometimes intensifying existing conditions. Gentle exercise, as advised by your doctor, can help manage this.
You might experience mood swings, including irritability or depression. Open communication with your doctor and support network is key during this time.
Some individuals notice increased appetite or weight gain. Maintain a balanced diet and consult your doctor or a registered dietitian for guidance.
Headaches are also possible. Over-the-counter pain relievers can offer relief, but check with your physician first.
A return of the original condition for which prednisone was prescribed is possible. This doesn’t necessarily indicate failure; your doctor will monitor and adjust the tapering schedule as needed.
Skin changes, such as thinning or bruising, can occur. Gentle skin care and avoiding harsh products can help.
Remember, these are potential symptoms; not everyone experiences them all, or experiences them to the same degree. Always discuss any concerns with your doctor.
Managing Symptoms During Tapering: Practical Tips
Record your symptoms daily. Note the time of day, symptom severity (using a scale of 1-10), and any triggers. This detailed log helps you and your doctor identify patterns and adjust the tapering schedule accordingly.
Communicate with your doctor regularly.
Don’t hesitate to contact your doctor if you experience worsening symptoms. They can help you manage flare-ups and potentially adjust your tapering plan. Open communication ensures your safety and comfort during this process.
Consider adding supportive therapies. Gentle exercise, like walking, can improve mood and reduce inflammation. Prioritize sleep; aim for 7-9 hours nightly. Stress management techniques, including meditation or deep breathing exercises, can also be beneficial. A balanced, nutritious diet supports your overall health and resilience.
Listen to your body.
Rest when you need it. Avoid strenuous activities during flare-ups. Pay attention to your body’s signals and adjust your activity level accordingly. Small changes can make a big difference in managing your symptoms.
Maintain a healthy lifestyle.
Hydration is key; drink plenty of water throughout the day. Avoid alcohol and excessive caffeine, which can exacerbate symptoms. A consistent sleep schedule promotes better rest and overall well-being.
Expect some discomfort.
Tapering is a gradual process. Some discomfort is expected. Focus on managing your symptoms effectively rather than expecting complete symptom absence throughout the process. Your doctor is there to help you navigate this.
Monitoring Your Progress and Consulting Your Doctor
Regularly track your symptoms. Keep a detailed journal noting any changes in your condition, including frequency and severity of symptoms for which you were prescribed prednisone. Note any new symptoms as well.
Schedule follow-up appointments with your doctor. These appointments allow for close monitoring of your progress and adjustment of the tapering schedule as needed. Don’t hesitate to contact your doctor between appointments if you have concerns.
Blood Pressure and Weight Monitoring
Monitor your blood pressure and weight at home. Significant fluctuations in either can indicate a problem and require immediate medical attention. Record these readings in your journal alongside your symptom tracking.
Important Signs to Report to Your Doctor
Report any of the following to your doctor immediately: severe fatigue, increased pain, significant weight gain or loss, increased thirst or urination, blurred vision, or muscle weakness.
Example of a Symptom Tracking Table
| Date | Symptom | Severity (1-10) | Blood Pressure | Weight | Notes |
|---|---|---|---|---|---|
| October 26, 2024 | Joint Pain | 7 | 120/80 | 155 lbs | Increased pain after exercise |
| October 27, 2024 | Joint Pain | 6 | 122/82 | 154 lbs | Slight improvement |
Communicating with Your Doctor
Be open and honest with your doctor about your experience. Accurate reporting of your symptoms ensures your doctor has the information needed to make the best decisions for your care. Your doctor will help guide you through the process.
When to Seek Immediate Medical Attention
Contact your doctor or go to the emergency room immediately if you experience any of the following:
Severe allergic reactions, including hives, swelling of your face, lips, or tongue, or difficulty breathing. These can be life-threatening.
Severe or worsening infections. Look for high fever, chills, worsening cough or other infection symptoms despite taking prednisone.
Sudden, significant weight gain. This can indicate fluid retention, a serious side effect of prednisone.
Intense muscle weakness or severe fatigue, significantly impairing your daily activities.
Increased blood pressure, accompanied by severe headache, blurred vision, or other symptoms of hypertensive crisis. Monitor your blood pressure regularly if prescribed.
Severe stomach pain or vomiting of blood, suggesting gastrointestinal bleeding.
Changes in mental status, including confusion, disorientation, or hallucinations. These can indicate a serious side effect.
Significant vision problems, including blurry vision or double vision. Report any changes promptly.
Unusual bruising or bleeding. This points to potential problems with blood clotting.
Seek medical attention if you experience any new or worsening symptoms during prednisone use, even if they seem minor. Don’t hesitate to contact your healthcare provider for any concerns.