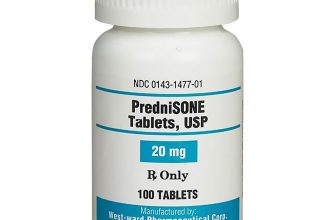
Prednisone, a common corticosteroid, can increase your heart rate. This effect, known as tachycardia, is often dose-dependent, meaning higher doses usually correlate with a faster heart rate. Monitor your pulse regularly while on prednisone, especially during dosage adjustments.
Several factors influence the likelihood of experiencing prednisone-induced tachycardia. Your individual sensitivity to the medication plays a significant role. Pre-existing heart conditions significantly increase the risk; discuss any cardiac history with your doctor before starting prednisone. Furthermore, dehydration can exacerbate the effect, so maintain adequate hydration.
Should you experience a rapid or irregular heartbeat (tachycardia) while taking prednisone, contact your physician immediately. They can assess the severity, adjust your dosage, or explore alternative treatment options. Never adjust your prednisone dosage without consulting your doctor. Your health care provider can monitor your heart rate and address any potential complications.
Remember: This information provides general guidance. Always consult your doctor for personalized advice regarding prednisone and your specific health situation. Prompt medical attention is crucial if you experience concerning symptoms.
- Tachycardia and Prednisone: Understanding the Link
- How Prednisone Affects Heart Rate
- Recognizing Tachycardia Symptoms
- Managing Tachycardia While on Prednisone
- When to Seek Immediate Medical Help
- Important Note
- What is Tachycardia?
- Causes of Tachycardia
- Symptoms Beyond a Rapid Heartbeat
- How Prednisone Works in the Body
- Anti-inflammatory Effects
- Immunosuppressive Actions
- Metabolic Effects
- Other Effects
- Prednisone’s Effect on the Cardiovascular System
- Increased Risk of Blood Clots
- Influence on Heart Rate
- Why Prednisone Might Cause Tachycardia
- Direct Effects on the Heart
- Indirect Effects
- Managing Tachycardia Related to Prednisone
- When to Seek Immediate Medical Attention
- Recognizing Tachycardia Symptoms While on Prednisone
- Common Symptoms of Tachycardia
- Less Common, but Serious Symptoms
- Managing Tachycardia Related to Prednisone Use
- Lifestyle Adjustments
- Medication Management
- When to Seek Immediate Medical Attention
- When to Consult a Doctor
- Prednisone-Specific Considerations
- Monitoring Your Heart Rate
Tachycardia and Prednisone: Understanding the Link
Prednisone, a common corticosteroid, can increase your heart rate, sometimes causing tachycardia. This isn’t always a cause for alarm, but it’s important to understand why it happens and what to do.
How Prednisone Affects Heart Rate
Prednisone’s mechanism involves increasing the body’s production of certain hormones. This hormonal surge can directly stimulate the heart, leading to a faster heartbeat. The extent of the increase varies; some experience only a minor elevation, while others may develop noticeable tachycardia. Factors like dosage, duration of treatment, and individual sensitivity influence this effect.
Recognizing Tachycardia Symptoms
Symptoms of tachycardia include a rapid or irregular heartbeat, often above 100 beats per minute. You may also experience palpitations (feeling your heart thumping), dizziness, shortness of breath, and chest pain. If you experience these symptoms, especially alongside prednisone use, seek medical attention immediately.
Managing Tachycardia While on Prednisone
Your doctor will assess your overall health and determine the best course of action. They might adjust your prednisone dosage, consider alternative medications, or recommend lifestyle modifications like regular exercise and stress management techniques. They may also suggest monitoring your heart rate at home using a heart rate monitor. Open communication with your doctor about your symptoms is paramount.
When to Seek Immediate Medical Help
Seek immediate medical attention if you experience severe or persistent tachycardia, chest pain, shortness of breath, or fainting. These can indicate a more serious underlying condition. Don’t hesitate to contact your doctor or seek emergency care.
Important Note
This information is for educational purposes only and does not substitute for professional medical advice. Always consult your doctor or other qualified healthcare provider before making any decisions related to your health or treatment.
What is Tachycardia?
Tachycardia is a heart rate exceeding 100 beats per minute (bpm) in adults. This rapid heartbeat can feel like a fluttering or pounding in your chest.
Causes of Tachycardia
Many factors can trigger tachycardia. Common causes include stress, anxiety, dehydration, fever, and certain medications, including prednisone. Underlying heart conditions, such as heart valve problems or abnormal heart rhythms, can also cause tachycardia. Sometimes, the exact cause remains unidentified.
Symptoms Beyond a Rapid Heartbeat
Besides a fast heartbeat, you might experience dizziness, shortness of breath, chest pain, and lightheadedness. The severity of symptoms varies greatly depending on the underlying cause and the individual’s health.
If you experience persistent or severe tachycardia, seek immediate medical attention. A doctor can perform tests to diagnose the cause and recommend appropriate treatment.
How Prednisone Works in the Body
Prednisone, a corticosteroid, mimics the effects of cortisol, a hormone your body naturally produces. It significantly impacts various bodily processes by binding to receptors inside your cells. This binding triggers a cascade of events, influencing gene expression and protein synthesis.
Anti-inflammatory Effects
Prednisone reduces inflammation by inhibiting the production of inflammatory chemicals like prostaglandins and leukotrienes. It also stabilizes lysosomal membranes, preventing the release of damaging enzymes. This action explains its effectiveness in treating conditions like asthma and arthritis.
Immunosuppressive Actions
Prednisone lowers the immune system’s activity. It decreases the number of circulating white blood cells and reduces the production of antibodies. This is beneficial in autoimmune diseases where the immune system attacks the body’s own tissues but can increase susceptibility to infections.
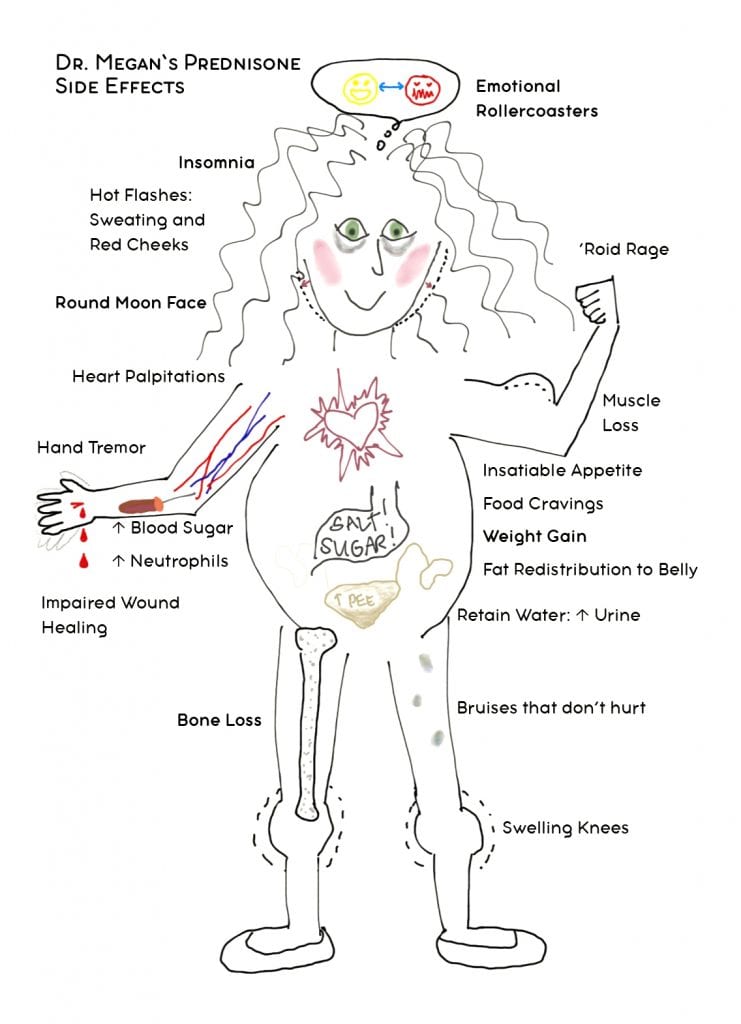
Metabolic Effects
Prednisone affects metabolism by increasing blood sugar levels (hyperglycemia) and influencing fat distribution. It can also affect bone density, potentially leading to osteoporosis with prolonged use. These metabolic changes necessitate close monitoring, particularly in patients with pre-existing conditions like diabetes.
Other Effects
Prednisone can influence fluid and electrolyte balance, potentially causing fluid retention and increased blood pressure. It can also affect the central nervous system, leading to changes in mood or behavior in some individuals. Always discuss potential side effects with your doctor.
Prednisone’s Effect on the Cardiovascular System
Prednisone, a glucocorticoid, can influence the cardiovascular system in several ways. It increases blood pressure through sodium and water retention and vasoconstriction. This effect is dose-dependent, meaning higher doses generally lead to more significant blood pressure elevation. Regular monitoring of blood pressure is crucial during prednisone therapy.
Increased Risk of Blood Clots
Prednisone also impacts blood clotting. It can increase the risk of developing blood clots (thromboembolism), particularly in individuals with pre-existing risk factors like obesity or immobility. Patients should be aware of symptoms like leg swelling, chest pain, or shortness of breath and report them immediately to their physician. Prophylactic measures, such as compression stockings or anticoagulants, might be considered depending on individual risk assessment.
Influence on Heart Rate
While not consistently observed, some patients experience an increase in heart rate (tachycardia) while on prednisone. This increase can be related to the medication’s effect on blood pressure or other underlying conditions. Careful monitoring of heart rate is advisable, particularly for individuals with pre-existing heart conditions.
It’s vital to remember that individual responses to prednisone vary. Always consult your doctor regarding any concerns or side effects experienced while taking this medication. They can assess your specific risk profile and tailor treatment accordingly.
Why Prednisone Might Cause Tachycardia
Prednisone, a corticosteroid, can increase your heart rate (tachycardia) through several mechanisms.
Direct Effects on the Heart
- Increased Heart Contractility: Prednisone enhances the force of your heart’s contractions. This stronger beat can lead to a faster heart rate.
- Sensitization to Catecholamines: Prednisone makes your heart more responsive to adrenaline and noradrenaline. These hormones naturally increase heart rate, and prednisone amplifies this effect.
- Electrolyte Imbalances: Prednisone can disrupt potassium levels. Low potassium (hypokalemia) is a known contributor to irregular heartbeats and tachycardia.
Indirect Effects
- Fluid Retention: Prednisone can cause the body to retain fluid, increasing blood volume. This increased volume places more demand on the heart, potentially raising heart rate.
- Blood Sugar Increase: Elevated blood sugar (hyperglycemia) from prednisone can indirectly stimulate the sympathetic nervous system, leading to a faster heartbeat.
Managing Tachycardia Related to Prednisone
- Consult your doctor: Discuss any concerning heart rate changes immediately. They can assess your specific situation and adjust your dosage or treatment plan.
- Monitor your blood pressure and heart rate: Regular monitoring can help detect problems early.
- Follow dietary guidelines: Maintain a balanced diet, avoiding excessive caffeine and alcohol, to minimize additional stress on your cardiovascular system.
- Lifestyle adjustments: Incorporate regular exercise and stress-reducing techniques to support overall cardiovascular health.
When to Seek Immediate Medical Attention
Seek immediate medical help if you experience rapid or irregular heartbeats accompanied by dizziness, chest pain, or shortness of breath.
Recognizing Tachycardia Symptoms While on Prednisone
Prednisone can increase your heart rate. Pay close attention to your body. If you notice any of the following, contact your doctor immediately.
Common Symptoms of Tachycardia
- A racing or pounding heart (palpitations)
- Heart rate consistently above 100 beats per minute (BPM) at rest
- Shortness of breath
- Lightheadedness or dizziness
- Chest pain or discomfort
- Fatigue or weakness
- Anxiety or nervousness
These symptoms can be subtle at first. Don’t ignore even minor changes in how your heart feels.
Less Common, but Serious Symptoms
- Fainting or near-fainting
- Severe chest pain
- Difficulty breathing
These indicate a more urgent need for medical attention. Seek help immediately.
Keep a record of your heart rate at different times of the day. This will assist your doctor in assessing your condition. Regular monitoring can help you and your doctor manage your medication effectively.
Managing Tachycardia Related to Prednisone Use
Monitor your heart rate regularly. Keep a record to track changes and share this information with your doctor. If your heart rate consistently exceeds 100 beats per minute (bpm) while resting, or you experience palpitations or shortness of breath, contact your physician immediately.
Lifestyle Adjustments
Maintain a healthy diet low in sodium and saturated fat. Regular, moderate exercise, such as brisk walking, can help. Avoid caffeine and alcohol, as these can stimulate your heart. Ensure adequate hydration by drinking plenty of water throughout the day. Stress reduction techniques, like deep breathing exercises or yoga, can also be beneficial. Prioritize sufficient sleep; aim for 7-8 hours nightly.
Medication Management
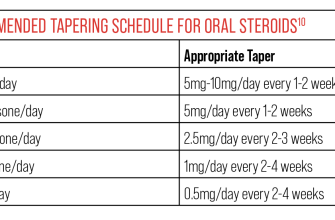
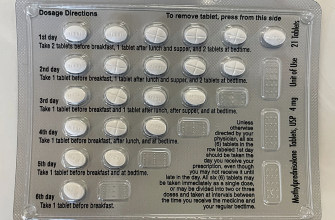
Your doctor might adjust your prednisone dosage. They may also prescribe beta-blockers or other medications to control your heart rate. Never stop taking or adjust your medications without consulting your physician. Open communication with your doctor is vital for effective management.
When to Seek Immediate Medical Attention
Seek immediate medical care if you experience chest pain, severe dizziness, fainting, or difficulty breathing alongside a rapid heart rate. These symptoms indicate a potential serious cardiac event requiring prompt intervention.
When to Consult a Doctor
Seek immediate medical attention if your heart rate exceeds 100 beats per minute (bpm) at rest, especially if accompanied by dizziness, shortness of breath, chest pain, or fainting. This is crucial, regardless of whether you’re taking prednisone.
Contact your doctor if you experience a sudden increase in heart rate, even if it’s only temporarily elevated. Note the duration and intensity of the increased heart rate, and any associated symptoms. This information helps your doctor assess the situation.
Prednisone-Specific Considerations
Prednisone can increase your heart rate. If you’re taking prednisone and notice a persistent increase in your heart rate, or if your resting heart rate consistently remains above 100 bpm, contact your doctor. They can adjust your dosage or evaluate potential interactions with other medications you may be taking.
Monitoring Your Heart Rate
Regularly monitoring your heart rate can be beneficial, especially if you’re taking prednisone. A simple method is to check your pulse for 60 seconds. Consider using a heart rate monitor or a fitness tracker for more accurate and continuous tracking.
| Symptom | Action |
|---|---|
| Resting heart rate consistently over 100 bpm | Contact your doctor immediately. |
| Sudden, significant increase in heart rate with symptoms | Seek immediate medical attention. |
| New onset of palpitations or irregular heartbeat | Contact your doctor. |
Remember, prompt medical attention is key to managing tachycardia. Don’t hesitate to contact your physician if you have any concerns about your heart rate, especially while on prednisone.