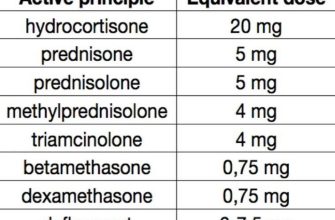
Gradually reduce Solumedrol dosage while simultaneously increasing prednisone to minimize withdrawal symptoms. A common tapering schedule involves decreasing Solumedrol by 25-50mg every 2-3 days, while concurrently increasing prednisone at a similar rate, aiming for equivalent anti-inflammatory effects. This ensures a smooth transition and prevents significant cortisol deficiency.
Close monitoring of your condition is crucial during this period. Report any new or worsening symptoms like fatigue, muscle weakness, or joint pain to your doctor immediately. Regular blood tests might be necessary to assess your cortisol levels and adjust the tapering schedule accordingly. Individual needs vary, so a personalized plan based on your specific health status and response to treatment is recommended.
Remember that the precise tapering regimen depends on your individual circumstances and your physician’s judgment. Factors such as the initial Solumedrol dose, the duration of treatment, and your overall health will influence the tapering strategy. Don’t hesitate to discuss your concerns and any changes in your health with your doctor to ensure you’re on the safest and most effective path.
Caution: Never abruptly stop taking Solumedrol or prednisone without consulting your physician. Sudden cessation can lead to severe withdrawal symptoms and complications. Always follow your doctor’s instructions precisely.
- Tapering Solu-Medrol to Prednisone: A Detailed Guide
- Understanding the Transition: Solu-Medrol vs. Prednisone
- Creating a Safe Tapering Schedule: Dosage and Timeline
- Monitoring for Side Effects and Managing Potential Complications
- Gastrointestinal Issues
- Bone Health
- When to Seek Medical Attention: Recognizing Warning Signs
- Monitoring Your Body: What to Watch For
- Additional Considerations
Tapering Solu-Medrol to Prednisone: A Detailed Guide
Consult your doctor to determine the optimal tapering schedule. They will consider your specific condition, medical history, and current dosage.
A common approach involves gradually reducing the Solu-Medrol dose while simultaneously increasing the Prednisone dose. This overlap ensures continuous corticosteroid coverage, minimizing withdrawal symptoms.
For example, a physician might suggest decreasing Solu-Medrol by 10-20mg every 3-5 days while simultaneously increasing Prednisone by a corresponding amount. Adjustments depend on your response.
Closely monitor yourself for withdrawal symptoms such as fatigue, muscle weakness, joint pain, nausea, or increased inflammation. Report any significant changes to your doctor immediately.
Blood tests may be necessary to monitor your cortisol levels throughout the tapering process. This helps your doctor ensure the transition is safe and effective.
The duration of the tapering process varies. It could take several weeks or even months, depending on individual needs. Patience and consistent communication with your healthcare provider are key.
Once the Solu-Medrol is discontinued, your doctor will likely continue to taper the Prednisone gradually. The tapering rate for Prednisone also depends on various factors. Be prepared for a prolonged tapering period.
Throughout this process, maintaining a healthy lifestyle – including proper diet, regular exercise (as tolerated), and adequate sleep – can improve your overall well-being and support your body during the transition.
Remember: This guide offers general information. Your doctor will create a personalized plan tailored to your situation. Always follow their specific instructions.
Understanding the Transition: Solu-Medrol vs. Prednisone
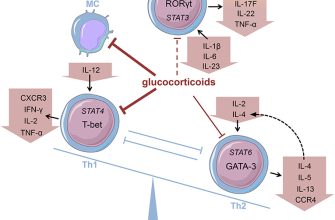
Solu-Medrol (methylprednisolone) is a powerful, fast-acting steroid given intravenously or intramuscularly, while prednisone is an oral steroid with a longer duration of action. Doctors often use Solu-Medrol for initial, rapid symptom relief in conditions like severe inflammation or allergic reactions. This is because it reaches peak effect much faster than prednisone.
The transition involves gradually reducing the Solu-Medrol dose as prednisone is introduced. This minimizes the risk of withdrawal symptoms. Your doctor will design a personalized tapering schedule based on your specific needs and response to treatment. Expect close monitoring of your condition during this phase. Regular blood tests and check-ups are standard practice.
Prednisone is often preferred for long-term management because it’s taken orally, making it more convenient. However, long-term prednisone use carries side effects, which makes careful monitoring and gradual dose reduction crucial. Always follow your physician’s instructions precisely and report any new symptoms immediately.
Common side effects of both medications include increased appetite, weight gain, mood changes, and insomnia. Long-term prednisone use can additionally lead to bone thinning and increased risk of infections. Discuss these potential issues and your concerns with your healthcare provider. They can help manage these risks with additional treatments or lifestyle adjustments.
Remember, individual responses vary. Open communication with your doctor throughout the transition period is vital for a safe and successful outcome. They will adjust the tapering plan as needed, based on your progress and well-being.
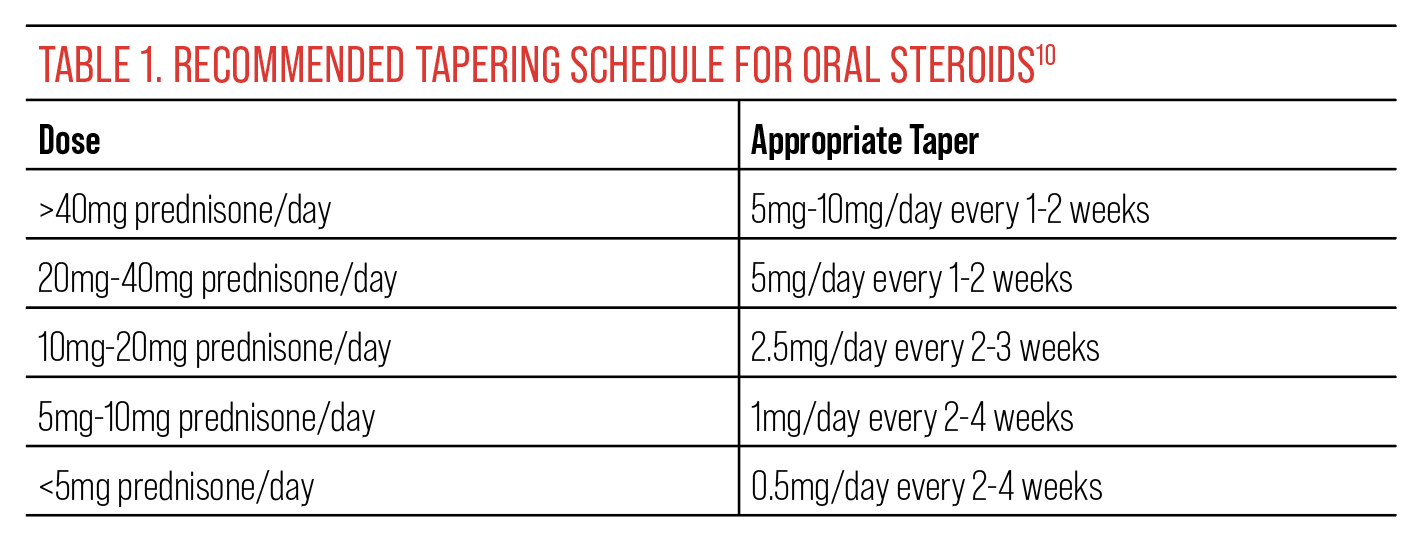
Creating a Safe Tapering Schedule: Dosage and Timeline
Begin by consulting your doctor. They will personalize a plan based on your specific needs and medical history. A common approach involves a gradual reduction, but the exact schedule varies greatly.
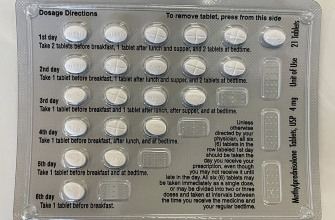
Here’s an example of a possible tapering schedule, but remember, this is not a prescription. Your doctor will adjust this based on your response:
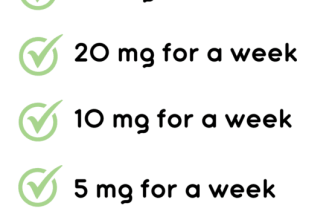
- Week 1-2: Reduce Solumedrol by 5mg daily. For example, if you are on 40mg, reduce to 35mg for a week, then 30mg.
- Week 3-4: Continue reducing by 5mg daily increments, transitioning to prednisone at the same daily dose.
- Week 5-8: Decrease prednisone dose by 2.5mg to 5mg every 3-7 days, depending on your tolerance.
- Week 9 onwards: Continue decreasing by smaller increments (1-2.5mg) until you reach a very low dose, or discontinue medication altogether. Your doctor might suggest alternating-day dosing to minimize side effects.
Important factors influencing the schedule include:
- Your initial dose of Solumedrol.
- Your overall health and response to treatment.
- Presence of any underlying conditions.
- Potential side effects experienced during the tapering process.
Closely monitor your symptoms throughout the process. Report any worsening symptoms to your doctor immediately. This might include increased inflammation, fatigue, or joint pain. Regular blood tests can help monitor your progress and adjust the schedule accordingly.
Remember, slow and steady is key. Rapid tapering can lead to serious withdrawal symptoms. Patience and careful monitoring are vital for a successful and safe transition from Solumedrol to prednisone.
Monitoring for Side Effects and Managing Potential Complications
Regularly monitor your blood pressure, weight, and blood sugar levels. Report any significant changes to your doctor immediately. These are common areas affected by both Solumedrol and Prednisone.
Pay close attention to your mood and mental state. Prednisone can cause mood swings, anxiety, or even depression. Don’t hesitate to discuss any emotional changes with your healthcare provider. They can offer strategies for coping and, if needed, prescribe additional medication.
Gastrointestinal Issues
Watch for signs of stomach upset, such as heartburn, nausea, or ulcers. Your doctor may recommend taking medications to protect your stomach lining or adjusting your dose. Maintain a healthy diet, and consider over-the-counter antacids if needed, always consulting your doctor first.
Bone Health
Long-term corticosteroid use can weaken bones. Increase your calcium and vitamin D intake through diet and/or supplements. Discuss the possibility of bone density testing with your doctor to monitor your bone health.
Report any unusual bruising, bleeding, or skin infections. These can indicate immune system suppression. Your doctor may adjust your medication or recommend preventive measures. Maintain good hygiene and promptly address any cuts or wounds to reduce infection risks.
Remember, open communication with your doctor is key to successful tapering and managing any potential complications. Don’t hesitate to contact them with any concerns or questions you may have. Proactive monitoring and timely intervention can help minimize side effects and ensure a smooth transition.
When to Seek Medical Attention: Recognizing Warning Signs
Contact your doctor immediately if you experience any of the following symptoms during your taper from Solumedrol to prednisone: Severe abdominal pain, vomiting, or bloody stools; Increased shortness of breath or chest pain; Significant weight gain (more than 2 pounds in a day); Severe muscle weakness; Severe headache or dizziness; Blurred vision; Severe swelling of your face, hands, or feet; Seizures; Changes in mental state, such as confusion or disorientation; Skin rashes or hives; High fever (over 101°F or 38.3°C); Unexplained bruising or bleeding.
Monitoring Your Body: What to Watch For
Pay close attention to your body’s response to the medication change. Keep a record of your daily weight, blood pressure, and any unusual symptoms. Report even subtle changes to your doctor. Regular communication is key to a safe and successful taper. Don’t hesitate to reach out – your health is the priority.
Additional Considerations
If you notice a sudden worsening of any pre-existing conditions, contact your physician immediately. For example, if you have a history of heart problems and notice increased palpitations or chest discomfort, do not delay seeking care. This also applies to worsening of conditions like diabetes or high blood pressure.